With Dr Jason Winnett, bariatric and laparoscopic surgeon
Whilst millions of people around the globe are embracing GLP-1 receptor agonists as the powerful new weapon in the war on obesity, compelling new evidence shows that surgery still sustains significantly greater weight loss1.
A study published in September 2025 in JAMA Surgery (Journal of the American Medical Association)1 involved more than 30,458 patients who were tracked for two years. It showed that patients who underwent metabolic bariatric surgery (MBS) achieved far greater and more durable weight loss than those treated with GLP-1 medications.
Surgery vs. weight-loss medications: which has better results?
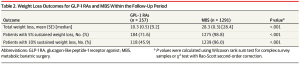
According to the JAMA study: after two years, 98.8% of surgical patients maintained at least a 5% reduction in their starting body weight, and 96% sustained a weight loss of 10% or more of their starting weight.
By comparison, among those using GLP-1 agonists, 71.6% maintained at least a 5% weight loss, and 45.9% achieved and sustained a 10% reduction.
The difference in total weight loss was also striking: after about two years, the surgical patients had lost an average of 28.3% of their starting body weight, while those treated with GLP-1s lost an average of 10.3%.
Source: JAMA, September 2025
Surgery vs. weight-loss medications: what’s the difference in cost?
Melbourne-based bariatric and laparoscopic surgeon Dr Jason Winnett concurs with the authors’ conclusion that surgical treatment may offer ‘greater effectiveness at a lower cost’ than obesity management medication for the durable treatment of obesity.
The JAMA study found that patients who had weight-loss surgery spent around US$11,869 USD (about AU$18,330) less on treatment compared with those using GLP-1 medications.
Despite the upfront costs of surgical treatment being higher at the beginning of the weight-loss journey, the ongoing expense of weight-loss medications quickly adds up. Over the two-year period, surgery not only delivered greater weight loss, but also ended up being more cost-effective.
‘Both of these treatments are game changers for patients,’ says Dr Winnett. ‘But we still need further studies to determine whether there are patient subgroups that would benefit from an earlier referral to surgery, particularly those with higher levels of obesity or people with obesity and diabetes (diabesity).’
How much do weight-loss medications cost?
According to the American JAMA study, weight-loss medications tend to cost around US$37,000 (approx. AU$56,990) over a two-year period. How does this compare in Australia where medications are significantly cheaper?
Semaglutide
In Australia, at a large chemist chain, semaglutide for weight loss currently costs about $250 per month at lower doses (.25mg and 0.5mg) or $6000 over two years.
At the higher doses (2.7mg), patients could pay about $370 per month or about $8800 over two years, with slight variations depending on the pharmacy of purchase.
Tirzepatide
Tirzepatide (Mounjaro), which was recently found to be slightly more effective than semaglutide (Ozempic and Wegovy) in a head-to-head study, also has a considerable monthly outlay.
Tirzepatide here in Australia is roughly $280 per month for a starting dose of 2.5mg or $690 per month for the highest dose.
Over two years, this would equate to $9,360 for a low dose or $16,800 for the high dose, again with slight variations depending on where it was purchased.
So, is surgery a better choice than weight-loss medications?
Dr Winnett says that for patients who do not want these large ongoing monthly costs, or who are severely overweight, surgery remains the optimal option for cost and effectiveness.
‘On the other hand, people with Class 1 obesity who often have only 5 or 10kg to lose may prefer the ongoing costs of GLP-1s. They can then try to taper 6 or 12 months after weight is stable, when exercise, sleep, and healthy eating habits are entrenched.
‘Although large studies show that for most GLP-1 patients, at least half the lost weight simply piles right back on 2 when they cease treatment, other studies show slow tapering of 2.5mg of semaglutide 3 can be successful.’
GLP-1 weight-loss medications: pros and cons
Weight loss is not the only upside of GLP-1s, according to a landmark 2024 New England Journal of Medicine study4.
Among the 3,533 participants with Type 2 diabetes, a three-year follow-up showed that those taking semaglutide had a 24% lower risk of a primary kidney event and an 18% lower risk of a major cardiovascular event.
‘But there are side effects, and the treatment of obesity is not like taking paracetamol to treat a cold, or an infection where you take antibiotics and you’re done,’ says Dr Winnett.
‘Obesity is a chronic disease, just like high blood pressure and diabetes. The patients who fare best are those who reach out early to their care team for help. Some people may need to stay on GLP-1s long-term.
‘And for people with “diabesity” or more complex or severe obesity, assessing the medical benefits of metabolic surgery early on is vitally important.’
Surgery vs weight-loss medications: risks and side effects
GLP-1s
The most common side effects of GLP-1 class receptor agonists include nausea, stomach pain, diarrhoea and constipation.
Very rare side effects, such as gastroparesis or failure of the stomach to empty, are usually resolvable, but of the millions who take GLP-1s, there are currently 2089 US lawsuits in October 2025. At the time of this article’s publication, no settlements have been reached.
Bariatric surgery
The risks of bariatric surgery are extremely low compared to previous decades.
‘Today, a bariatric surgery procedure has a similar safety profile to any other standard operation like a knee or hip replacement,’ says Dr Winnett.
The current Bariatric Surgery Register 2024 shows that since the registry started, there has been a total mortality rate of 70 per 178,000 bariatric surgeries in Australia5.
‘The risk of NOT having bariatric surgery for severely obese people means a much greater risk of premature death,’ says Dr Winnett. ‘This is especially in younger people (20-39 age group), where research shows that years of life lost (YLL) due to obesity are 8-10 years on average.6
Choosing your path to weight loss
While both GLP-1 medications and surgery can be effective for weight loss, the evidence continues to show that metabolic surgery delivers greater, longer-lasting results, and often at a lower overall cost.
While surgery is the more effective and durable option, GLP-1s provide a valuable alternative for those seeking a non-surgical approach.
Dr Winnett encourages anyone considering weight loss to seek professional guidance to find the approach that best suits their needs and long-term goals. ‘Health professionals are not only helpers on the weight loss journey, but importantly, they’re also listeners to help patients and answer questions. So never be afraid to ask!’
If you’d like to explore whether bariatric surgery is right for you, please get in touch with the Winnett Specialist Group.
P (03) 9417 1555 admin@winnettspecialistgroup.com.au
www.winnettspecialistgroup.com.au
Queens Terrace, 382 Victoria Parade, East Melbourne 3002
Sources
1 Obesity Treatment with Bariatric Surgery vs GLP-1 Receptor Agonists
2 Weight gain after stopping new obesity drugs, Science alert
4 Effects of Semaglutide on Chronic Kidney Disease in Patients with Type 2 Diabetes