
Nutrient Deficiencies in Bariatric Surgeries
Pre-existing and Postoperative Nutritional Deficiencies in Bariatric Patients
Nutrition education and medical nutrition therapy are integral to the success of a patient’s bariatric surgery journey. Nutrition counselling plays an especially important part in long-term weight loss maintenance, but it also serves to correct any pre-existing nutritional deficiencies or for any that come about after surgery. This article summarises nutritional deficiencies common to bariatric patients prior to and after surgery.
Pre-existing nutritional deficiencies
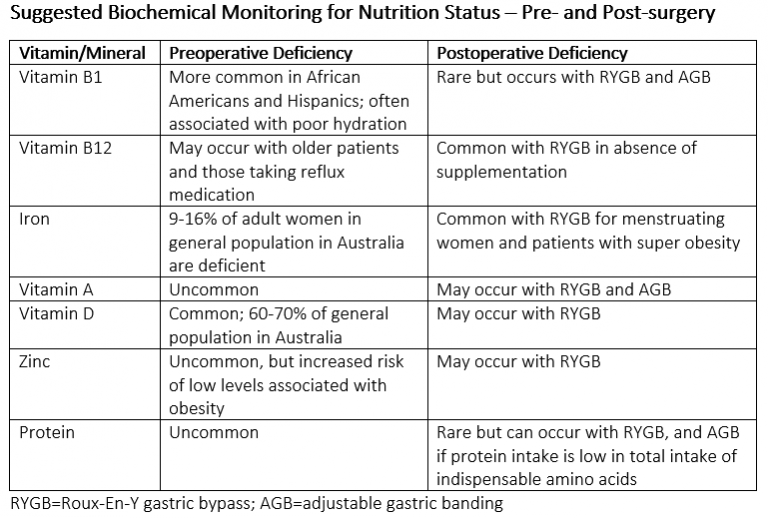
Some of the vitamin and mineral deficiencies we see in bariatric patients prior to their surgery include vitamin D, iron, zinc and vitamin B12. These could be due to a number of reasons including not getting enough sunlight (Vitamin D) or dietary sources of the nutrients, or there may be a physiological cause leading to poor absorption of these nutrients. Obesity is an inflammatory disease and inflammation can interfere with metabolic processes. The table below summarises nutritional deficiencies prior to and post-surgery in bariatric patients.
Why are nutrients at risk after surgery?
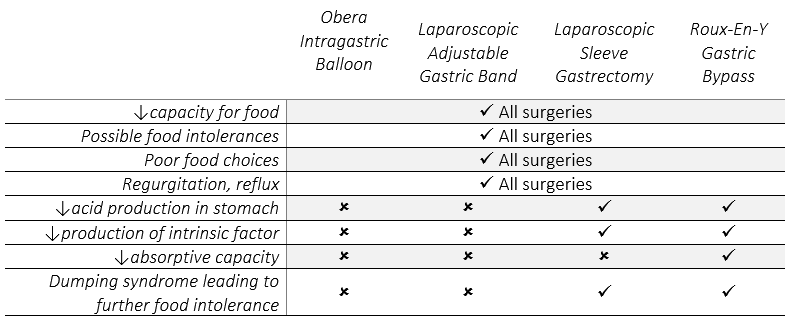
There is an increased risk of nutritional deficiencies with all types of bariatric surgery. This is due to several reasons including a reduced capacity for food, possible food intolerances coming about after surgery, poor food choices and occurrences of regurgitation or reflux. Some bariatric procedures are associated with a higher risk of nutritional deficiencies than others. While the Obera Intragastric Balloon and Laparoscopic Adjustable Gastric Band (LAGB) do reduce capacity for food and can be associated with the previously mentioned reasons for nutritional deficiencies, they do not alter human anatomy and physiology. The Roux-En-Y Gastric Bypass (RYGB) and Laparoscopic Sleeve Gastrectomy (LSG) both result in altered human anatomy and physiology, by which they help to contribute to weight loss, but may thus result in nutritional deficiencies. Some reasons behind the increased risk for nutritional deficiencies in the RYGB and LSG include reduced acid production in the stomach and the reduced production of a substance called intrinsic factor, which enables the body to absorb vitamin B12. Dumping syndrome or abnormally rapid bowel evacuation can occur with the RYGB and LSG
and this can cause nutritional deficiencies if it leads to food intolerance. Following is a table of how common types of bariatric surgery may or may not contribute to nutritional deficiencies.
Monitoring and Correcting Nutritional Deficiencies
It is essential for bariatric patients to work with a Dietitian or Physician to correct nutritional deficiencies and to optimise their nutrition status. Together with their multidisciplinary health team, patients should monitor their nutrient levels at 6 months, 12 months and 18 months postoperatively. These regular check-ups not only give your healthcare team the opportunity to correct any nutritional deficiencies which may occur, but reconnecting with and being accountable to your Dietitian and Physician will greatly contribute to the success of your weight loss journey.



