For many patients the decision to have bariatric surgery is a no-brainer.
You’ll look better. You’ll feel better.
You’ll reduce your risk of knee surgery.
And you’re significantly less likely to die behind the wheel*1 due to sleep apnoea.
Your sleep will improve, you’ll have a significantly reduced risk of Alzheimer’s, diabetes, asthma and other chronic diseases.
Intimacy will be back on the cards, and you’ll be able to chase your kids or grandkids around the house again.

But while many people find it easy to make the first step to have surgery – the second big decision is trying to understand which surgery is optimal.
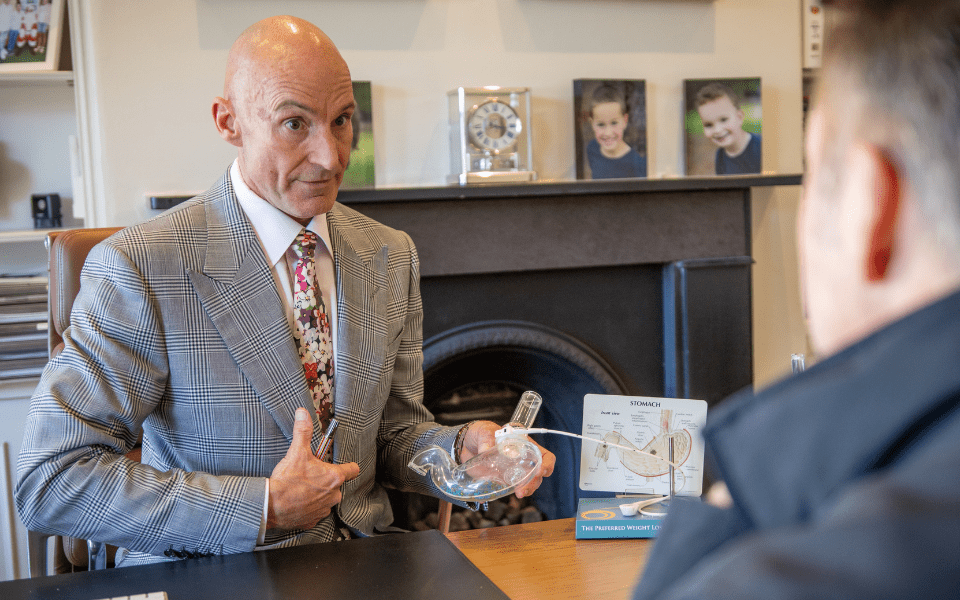
“The two questions I get asked the most from patients are which is the most effective surgery and which is the safest surgery,” says Mr Jason Winnett, Melbourne Laparoscopic and Bariatric Surgery.
“Because the Laparoscopic Sleeve Gastrectomy is a simpler procedure and takes less time on the operating table there has been a perception in years past that it may be slightly less risky than the Roux-en-Y Gastric Bypass Surgery.“
“However, this 2024 study finally provides definitive evidence that both procedures have an equal safety record.”
The findings, reported in the Journal of the American Medical Association involved 1735 post-bariatric surgery patients, and is the largest of its kind in the world.*2
At 30 days after surgery, both groups had few complications such as haemorrhage, leakage, blood clots and infections. There were no deaths in the 90-day follow up period.
“This is good news for doctors and patients alike because it means there is more choice without having to weigh up short-term surgical risks,” says Mr Winnett.
“This adds further weight to the notion that surgery outcomes have significantly improved based on 30 years of data.”
“Today morbidity and mortality is about 0.03 to 2% annually – in a cohort of patients that otherwise face a very high risk of premature death due to their obesity.”
Here are the main differences between the two procedures.
The Gastric Sleeve (Laparoscopic Sleeve Gastrectomy or LSG)

“The Sleeve is the go-to surgery for most uncomplicated bariatric patients,” says Mr Winnett. “It involves removing 75% of the stomach and converting to a banana shaped sleeve.”
“The LSG reduces appetite significantly by changing metabolic drivers in the brain and now with BMI requirements changing in 2022 for the first time in 30 years,*3 more Australians than ever are eligible to have the procedure.”
The current eligibility criteria for Sleeve Surgery is 30 with co-morbidities and 35 with no co-morbidities (e.g. diabetes, hypertension or sleep apnoea).
Mr Winnett also says LSG involves 2-3 days in hospital, healing time two weeks, return to routine in three weeks.
“The Sleeve also has less chance of Dumping Syndrome (which causes diarrhea, nausea) and many patients permanently go off diabetes medications and blood pressure medications after surgery.”
Gastric Bypass Surgery (Roux-en-Y Gastric Bypass)
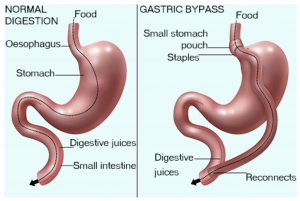
Photo source: healthdirect.gov.au
In the Gastric Bypass procedure, a small stomach pouch is created to restrict food intake.
The next stage of the operation involves a Y-shaped section of the small intestine being attached to the pouch to allow food to bypass the lower stomach, the duodenum (the first segment of the small intestine), and the first portion of the jejunum (the second segment of the small intestine).
This bypass reduces the absorption of nutrients and thereby reduces the kJ intake and increases satiety.
“Like sleeve surgery, this is a “metabolic” surgery that also impacts the brain’s hunger drivers,” says Mr Winnett.
“The new change in BMI requirements*3 for Gastric Bypass Surgery mean that a person with a BMI of 30 with co-morbidities (e.g. hypertension, sleep apnoea or diabetes) and 35 with no co-morbidities will be eligible for surgery.”
“The Bypass is also reversible, whereas the LSG is not, although it can later be converted to a bypass,” says Mr Winnett.
He says Bypass surgery is also often more suitable for patients with severe diabetes and reflux issues and tends to result in slightly more weight loss.
At Winnett Specialist Group, we understand that choosing the right bariatric surgery is a big decision. That’s why we offer a comprehensive pre-operative program.
You’ll meet with both your surgeon and a dietitian twice before surgery, as well as any necessary specialists, such as cardiologists, respiratory physicians, endocrinologists, clinical psychologists and/or psychiatrists as required.
Throughout your weight loss journey, our team will provide ongoing support with diet and exercise, ensuring you have the tools you need to succeed.
Contact Winnett Specialist Group today to learn more about how we can help you achieve your weight loss goals and improve your overall health.

Mr Jason Winnett
Laparoscopic and Bariatric Surgeon
P (03) 9417 1555
admin@winnettspecialistgroup.com.au
www.winnettspecialistgroup.com.au
Queens Terrace, 382 Victoria Parade, East Melbourne 3002
Sources
1 Obesity and Risk for Death Due to Motor Vehicle Crashes – PMC (nih.gov)
3 After 30 Years — New guidelines for weight loss surgery – Australian Associated Press (aap.com.au)