Managing weight is a personal journey that can have a powerful impact on long-term health, confidence, and quality of life. Today, there are more options than ever to support weight loss, including bariatric surgery and newer medications like GLP-1 receptor agonists (for example, Semaglutide, known by brand names like Ozempic® and Wegovy®).
Each approach offers important benefits, but also comes with its own considerations around effectiveness, costs, potential side effects, and long-term outcomes.
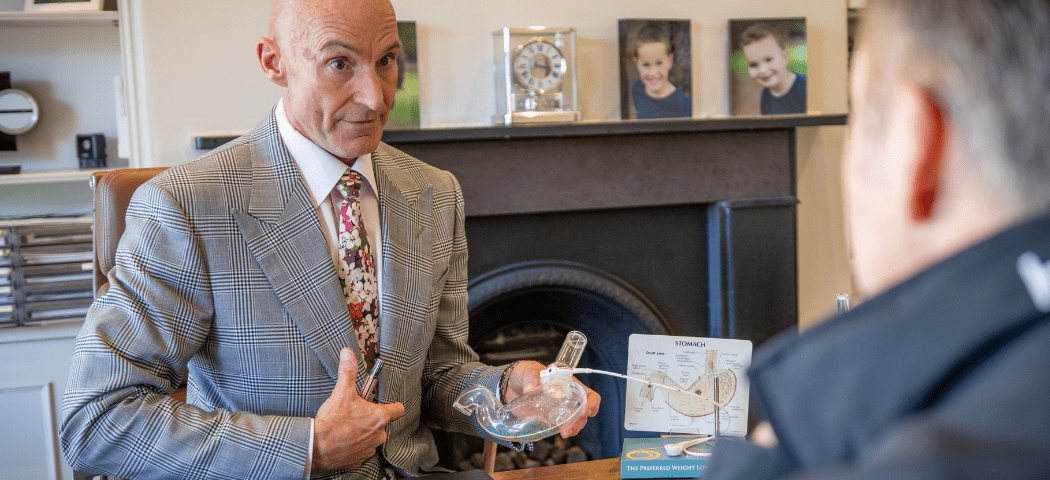
In this article, laparoscopic and bariatric surgeon Mr Jason Winnett shares his clinical insights into both treatments. We also share two real-life patient experiences that highlight the different paths individuals can take when working towards their health and wellbeing goals.
*All patient stories are shared with consent and provided for general information purposes only. They are not intended as endorsements of any specific treatment, and medical advice should always be sought from a qualified professional.
Megan’s Story: Choosing Surgery for Sustainable Change

‘I don’t want to pay $400 a month.’
Megan, 38, nurse and mum of three from Melbourne
Intervention: Gastric sleeve surgery in August 2023
Weight drop: 105kg to 75kg
Impact: Improved energy, better sleep, more confidence, and more time for her children.
‘When I embarked on my weight-loss journey, I never imagined how transformational it would be – not just for my body, but my mind and my spirit. I had put on a fair bit of extra weight after my last baby four years ago.
‘Having surgery was a giant leap of faith, but in reality, the procedure itself was not difficult. I was in hospital for two days and had a little bit of gas pain for about a week, but that was about it for the surgical aspect, along with slight pain around the five small incision scars (about 2cm each).
‘I had never consumed alcohol much at all, so not drinking was not a problem for me. I knew that things would only get worse with age and menopause.
‘At the time, I was nervous about not being able to control my hunger after surgery. In decades past, even as a child and teenager, I had always been big and always struggled to control my urges to eat! But the wonderful thing about surgery is that it helps to control your brain’s hunger signals.
‘I did consider weight-loss medications but was worried about side effects and wanted something more permanent. I also didn’t like the idea of paying more than $400 a month for injections for the rest of my life, because the reality is that if you stop taking the drugs, the weight piles back on.
‘I lost the bulk of my weight in the first six months of surgery and just a few kilograms per month in the past two months, but am now pretty close to my goal weight of 68kg.
‘With every kilogram lost, I suddenly had better health, more self-confidence, more energy for my kids, improved sleep, and could finally walk into a shop and know that I could find clothes to fit!’
Clinical Perspective: Surgery and Weight Management Outcomes
‘Weight-loss surgery is a very different concept in 2025 than it was a few decades ago,’ says Melbourne Bariatric Surgeon Mr Jason Winnett.
‘What was once considered a high-risk procedure is just as safe as a knee replacement surgery today. Scars are much smaller, and patients are generally walking on the same day.
‘Patients often ask me which way they should go. Some are better candidates for medication, and others for surgery. Surgery continues to be one of the most effective long-term treatment options for patients with severe obesity, while medications may be more suitable for individuals seeking a modest weight reduction of around 5–10 kilograms.’
A recent systematic review between 2020 and 2024 of 20,000 patients presented to the American Society for Metabolic and Bariatric Surgery showed:
- Diet and exercise alone achieved 7.4% weight loss, but the weight was generally regained within four years.
- Five months of weekly injections of GLP-1 semaglutide resulted in 10.6% weight loss, and nine months of tirzepatide 21.1% weight loss. However, once treatment was stopped, half the lost weight returned within a year.
- Metabolic and bariatric surgery, such as gastric bypass and sleeve surgery, demonstrated total weight loss of 31.9% and 29.5% after one year post-operation, with weight loss of approximately 25% maintained for up to 10 years.
‘What people with obesity need to ask themselves is: What are the risks of NOT having the surgery or weight-loss medications?’ says Mr Winnett. ‘Obesity has very clear links with cancer, sleep apnoea and increases the risk of arthritis significantly. After surgery, many of these risks drop significantly and Type II diabetes resolves permanently in most cases.’
Susan’s Story: Finding Success with GLP-1 Medications

Susan, 71, grandmother of eight and great-grandmother of one, from Wangaratta, Victoria
Treatment: Saxenda®, Ozempic®, Mounjaro®, Wegovy®
Weight drop: 76kg to 56kg
Impact: Improved metabolic health, increased energy, and confidence to enjoy an active life with her grandchildren.
‘Like many women, I noticed the weight started to creep up after menopause and before I knew it, I was 20kg heavier! I had also had my thyroid removed not long after that and have no doubt that was involved too.
‘My daughter’s wedding gave me the incentive I needed to do something about it.
I have eight grandchildren and play an active part in their lives and wanted to regain my strength and energy. Being overweight just made it that much more difficult.
‘My doctor and I together decided to start with Saxenda® and had some success, but then moved on to semaglutide (Ozempic®) which I felt yielded faster results. During the Ozempic® shortage I moved to Mounjaro®, and then semaglutide came in the form of Wegovy® recently. This is the sister drug of Ozempic® – the same ingredient but at a higher dose, designed specifically for weight loss.
‘However, I didn’t like it quite as much due to increased nausea, so I went back to Mounjaro®. The drug costs me $400 a month but in my mind is worth every cent. I eat less food, buy less food, but most of all my blood tests have improved so much metabolically speaking – with good cholesterol, liver, kidney and, in fact, all readings.
‘These days, I do about nine hours a week of line dancing for exercise and feel that as an older person, I am living ‘my best life’ and look and feel great!
‘I even went on the big slide with the grandkids in a cossie – something I would never have dreamed of doing a few years ago. I haven’t experienced any side effects apart from very mild nausea at the beginning, and my friends and family are amazed at my weight loss.’
The downsides?
‘I know that I may put the weight straight back on if I stop the medication, but I take it for health reasons, given that being overweight increases the risk factor for many different cancers and also arthritis.
‘I am grateful for medical supervision and being able to lose weight in a supportive environment.’

Susan lost 8kg in December 2022 and by 2025 had lost 20kg on weight-loss drugs.
Clinical Perspective: The Role of GLP-1 Medications
‘There is no doubt that semaglutide and other weight-loss drugs are a powerful tool for weight loss,’ says Mr Winnett. ‘Given that only a very small percentage of people who need weight-loss surgery are actually getting it in Australia, these drugs show great promise.
‘These medications also help keep blood sugar under control for patients with diabetes. We use them pre-surgery in some cases to enhance weight loss, to make it easier and safer to navigate through less fat and reduce liver bulk.’
New evidence in the New England Journal of Medicine found that among 3533 participants with Type II diabetes followed for 3.4 years, those treated with semaglutide had a 24% lower risk of experiencing a primary heart or kidney event compared to those who didn’t receive the treatment.
‘These studies show us that for people with diabetes, there is a significant reduction in risk of heart attack and kidney disease with semaglutide,’ says Mr Winnett.
He notes that other evidence suggests semaglutide may lower the risk of alcoholism and quell the desire to drink alcohol, as reported in New Scientist Magazine.
But what are the downsides?
‘We know that a lot of the lost weight just piles back on, and also side effects are not insignificant,’ Mr Winnett says. ‘Common side effects included diarrhoea and nausea, and there were some serious gastrointestinal side effects (9.8% in control group v 6.4% in placebo).’
There have also been links to temporary vision loss according to the American Academy of Ophthalmology.
Semaglutide has also more recently been linked to the stomach-paralysing condition gastroparesis, which has resulted in more than 1600 personal injury lawsuits in the US.
Mr Winnett says that some recent medical evidence shows that stopping medication may result in improvement or cessation of gastroporesis, as reported in the Journal of Investigative Medicine.
‘Gastroparesis disrupts regular, spontaneous muscle movements in the stomach,’ says Mr Winnett.
‘This prevents proper stomach emptying and can be very uncomfortable and cause symptoms of feeling full, vomiting, weight loss, tummy pain and bloating. It tends to be a chronic and painful disease. Whilst not usually life-shortening and it’s a condition that can be managed, we can’t expect that it will always be cured.
‘Any side effects must be carefully considered and weighed up against the “side effects” of not taking medications. This includes premature death for the morbidly obese as well as increased risk of heart attacks, cancer risk, joint pain, immobility, infertility and depression.’
Mr Winnett also recommends that semaglutide should be prescribed and used judiciously.
‘Ozempic is now also only prescribed for patients with Type 2 diabetes, while Wegovy® (same ingredients but stronger version of semaglutide) is for people without diabetes who want to lose weight. Other drugs in this class of GLP-1 agonists include Mounjaro® which has a similar weight loss to semaglutide.’
- At the Winnett Specialist Group, patients are seen by both surgeon and dietitians twice pre-operatively, as well as specific specialists such as cardiologists, respiratory physicians, endocrinologists, clinical psychologists and/or psychiatrists as required.
- All patients will receive dietetic and psychological support throughout their weight-loss journey at the Winnett Specialist Group.
- Follow-up with Winnett Specialist group surgery is 3-monthly and lifelong.
*Disclaimer: Information shared about procedures, treatments, or medications, including weight-loss medications, is intended for general information only and is not a substitute for personalised medical advice. Surgical and medical procedures carry risks, and we strongly recommend consulting a qualified health professional before making decisions. All content is published with patient consent and adheres to AHPRA and relevant regulations.

Mr Jason Winnett
Laparoscopic and Bariatric Surgeon
P (03) 9417 1555 admin@winnettspecialistgroup.com.au
www.winnettspecialistgroup.com.au
Queens Terrace, 382 Victoria Parade, East Melbourne 3002
Sources: Body mass index and ovulatory infertility – PubMed
Obesity and Risk for Death Due to Motor Vehicle Crashes – PMC
180812-Arthritis-Australia_submission-to-Obesity-Inquiry.pdf
Modest weight loss reduces breast cancer risk, Asco Post, 2018
Weight loss and blood pressure control, Hypertension Journal.
Medication induced gastroporesis, a case report, the Journal of Investigative Medicine 2021



