
Melbourne Laparoscopic and bariatric surgeon Mr Jason Winnett offers the latest insights on the world’s biggest safety study into bariatric surgery, released in 2024.
GPs play a crucial role in the management of obesity and recent 2022 revisions to BMI guidelines now allow more patients in Australia to meet eligibility criteria for life-changing bariatric surgery than ever before.
“Which surgery is the safest?” is a common question GPs and specialists will hear from their patients,” says Mr. Winnett.
“This new study in the Journal of the American Medical Association was a post-surgery study of 1735 patients, the largest of its kind and provides enlightening evidence for GPs and specialists alike.”
At 30 days after surgery, both the LSG and Bypass groups had few complications such as haemorrhage, leakage, blood clots and infections.
“Furthermore, there were no deaths in the 90-day follow up period.”
“This is good news for doctors and patients because it means there is more choice without having to weigh up short-term surgical risks.” risks, Mr Winnett says.
While Intragastric balloon and the mini-gastric bypass remain procedures that are growing in popularity for Class 1 obesity, LSG and the Roux-en-Y Gastric Bypass remain the procedure of choice for Class II and III obesity patients.
Here are the main differences between the two procedures.
The Gastric Sleeve (Laparoscopic Sleeve Gastrectomy or LSG)

“The Sleeve is the go-to surgery for most uncomplicated bariatric patients,” says Mr Winnett. “It involves removing 75% of the stomach and converting it to a banana shaped sleeve.”
“The LSG reduces appetite significantly by changing metabolic drivers in the brain and now with BMI requirements changing in 2022 for the first time in 30 years, more Australians than ever are eligible to have the procedure.”
The current eligibility criteria for Sleeve Surgery is 30 with co-morbidities and 35 with no co-morbidities (e.g. diabetes, hypertension or sleep apnoea).
Mr Winnett also says LSG involves 2-3 days in hospital, healing time two weeks, return to routine in three weeks.
“The Sleeve also has less chance of Dumping Syndrome (which causes diarrhea, nausea), and many patients permanently go off diabetes medications and blood pressure medications after surgery.”
Gastric Bypass Surgery (Roux-en-Y Gastric Bypass)
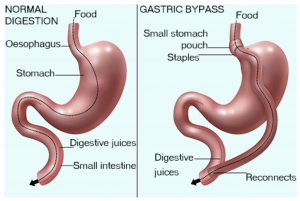
Photo source: healthdirect.gov.au
In the Gastric Bypass procedure, a small stomach pouch is created to restrict food intake.
The next stage of the operation involves a Y-shaped section of the small intestine being attached to the pouch to allow food to bypass the lower stomach, the duodenum (the first segment of the small intestine), and the first portion of the jejunum (the second segment of the small intestine).
This bypass reduces the absorption of nutrients and thereby reduces the kJ intake and increases satiety.
“The Bypass is also reversible, whereas the LSG is not, although it can later be converted to a bypass,” Mr Winnett says.
He says Bypass surgery is also often more suitable for patients with severe diabetes and reflux issues and tends to result in slightly more weight loss.
GP considerations for bariatric surgery
Investigations should include:
✓ Routine labs. It can include fasting lipids, full blood count, urea and electrolytes, liver function tests, coagulation screen, urinalysis, fasting glucose and glycated haemoglobin (HbA1c) for diabetes screening.
✓ C-peptide level to predict diabetes remission.
✓ Nutritional screen: iron studies, vitamin B12 folate 25-OH, vitamin D.
✓ Gastrointestinal evaluations, such as abdominal ultrasound and endoscopy may be required.
✓ Electrocardiogram and polysomnography may be required if cardiovascular or sleep apnoea is suspected.
✓ Psychiatric evaluation and psychiatry referral if known or suspected psychiatric illness or substance abuse.
✓ While there are today no absolute contraindications to bariatric surgery, relative contraindications for the more extensive surgeries such as sleeve and bypass do exist including heart failure, unstable coronary artery disease, end-stage lung disease, drug and alcohol dependency, impaired intellectual capacity and Crohn’s Disease (for BYPASS)
At the Winnett Specialist Group, patients undergo thorough evaluations with surgeons and dietitians before surgery. We also coordinate with specialists like cardiologists, respiratory physicians, endocrinologists, and psychologists or psychiatrists as needed.
Continued support doesn’t end post-operatively. Patients receive ongoing guidance in diet and exercise throughout their weight loss journey with us, as well as follow-up appointments every three months and lifelong.
For more information on bariatric surgery and weight loss support, visit our insights section or contact us directly. We’re here to share our knowledge with fellow health professionals and work together to enhance patient care. Reach out to us, and let’s improve patient outcomes together.
Mr Jason Winnett
Laparoscopic and Bariatric Surgeon
www.winnettspecialistgroup.com.au
Queens Terrace, 382 Victoria Parade, East Melbourne 3002
References:
1 Obesity and Risk for Death Due to Motor Vehicle Crashes – PMC (nih.gov)
3 After 30 Years — New guidelines for weight loss surgery – Australian Associated Press (aap.com.au)




