
The dataset for dementia in Australia paints a gloomy outlook. In Victoria alone there are 107,000 of our patients living with dementia today – a figure that will increase 101% by 2054*1, according to Dementia Australia predictions.
Dementia is now the leading cause of death in Australian women*2, and the second leading cause of death in men*3, according to the Australian Institute of Health and Welfare.
We also know that 40% of dementia factors are modifiable*4 and the take home message is that these lifestyle changes are particularly vital in mid-life.
Head injury, hearing loss, smoking and alcohol use are all well-known factors for dementia, however weight gain is increasingly gaining traction as a significantly modifiable risk factor.
For doctors it is often tricky to understand the schizophrenic spectrum of weight and cognitive decline.
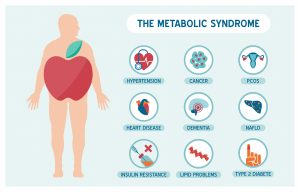
On the other hand, a lot of new research is pointing to the fact that preventing neurodegenerative changes in the first place can make a difference for obese patients, who are at significantly higher risk of developing dementia as part of the metabolic syndrome.
In one study of more than 6582 patients in the UK, reported in the International Journal of Epidemiology*6, women with central weight obesity had a 39% increased risk of dementia.
Other Cureus research*7 suggests that obesity-triggering vascular dementia decreases not only blood supply to the brain, but also increases fat cells that damage the brain’s white matter, leading to a loss of cognitive and intellectual behaviour.
While vascular dementia often impacts the fragile vessels in the brain and the fastest, more and more evidence is emerging that the neurodegenerative pathways in the brain have an impact on all three diseases*8 – obesity, diabetes and Alzheimer’s.
One JAMA study of more than 10,000 patients*9, also found that the earlier the onset of diabetes, the higher the risk of subsequent dementia.
What is my top takeaway from this then for GPs?
Obesity is a very complicated illness. I quite often tell patients that if they don’t have bariatric surgery, their knee pain will most likely not improve, or that their sleep apnoea will get worse.
But often it’s telling people about the real risk to brain health and loss of cognitive function is when it hits home hard.
The good news is that GPs can make a big difference by targeting weight loss changes in midlife or even earlier, rather than when BMI is higher in the later years of life*10.”
Recent research on bariatric patients also shows that executive function improved after sleeve or gastric surgery*11.
“While one marker (recall decline) suggests the need for further studies to look at these issues, overall cognition remained stable over two years, which is what we want to see given that obese individuals are at a higher risk of experiencing a faster rate of decline than those with a healthy weight.”
Another JAMA study on 133 bariatric patients, mostly women*12, found that post two years bariatric surgery
✓ 11% of participants improved working memory by 11%
✓ 31% demonstrated improvements in episodic memory.
✓ 24% showed improvement in verbal fluency.
✓ 40% were better able to shift their attention.
As GPs, your proactive approach to weight management can significantly mitigate the risk of cognitive decline in patients. To access detailed strategies and learn more about bariatric surgery and other weight management options, click here to explore our insights section at Winnett Specialist Group. Together, we can improve patient health outcomes.
Mr Jason Winnett
Laparoscopic and Bariatric Surgeon

Dr. Audrey Kotzander
Bariatric Physician
P (03) 9417 1555 admin@winnettspecialistgroup.com.au
www.winnettspecialistgroup.com.au
Queens Terrace, 382 Victoria Parade, East Melbourne 3002
References:
1, 2,3 Dementia in Australia Report 2024-2054
4 Brain health and risk reduction the GP role, RACGP
5 Alzheimer’s Disease and Weight Loss – Why it happens, Cleveland Clinic
7 Does obesity increase the risk of dementia?, Cureus May 2018
8 Common neurodegenerative pathways in obesity, diabetes, and Alzheimer’s disease, Science Direct 2018
9 Association Between Age at Diabetes Onset and Subsequent Risk of Dementia, JAMA 202,
12 Long-Term Brain Structure and Cognition Following Bariatric Surgery, JAMA 2024




