After months of hard work and successful weight loss, it can be frustrating and overwhelming to see the scales get “stuck”. This is a common challenge, known as a patient plateau, that many face after surgery. The Winnett Specialist Group team understands this struggle and offers 15 multidisciplinary ways to help you get the scales moving again.

1. Realise JUST 1kg a week can be OK…
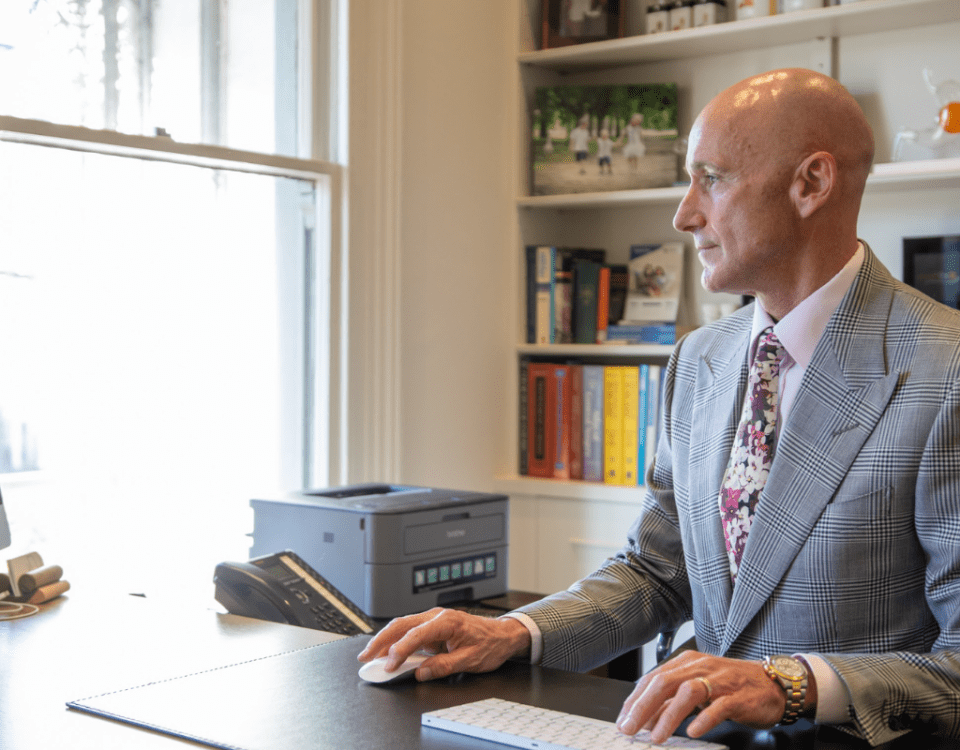
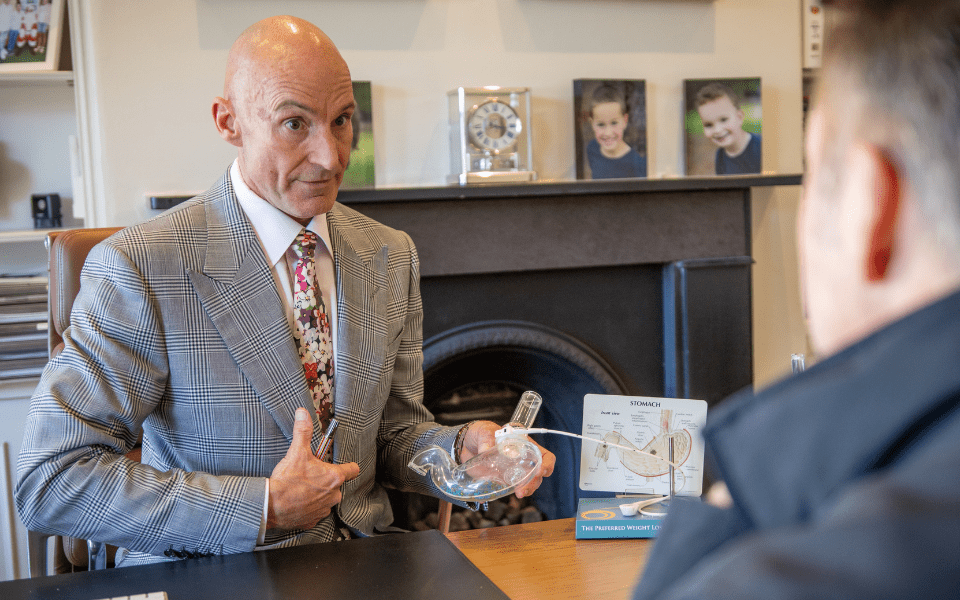
“Most weight loss occurs in the first 6-9 months post-surgery, and weight loss still continues for 12 months and then stabilises,” says Mr Jason Winnett, laparoscopic and bariatric Surgeon at the Winnett Specialist Group.
“One thing I have noticed with many patients is that this initial weight loss can be rapid, and this can sometimes give patients an unrealistic sense of how much weight loss is possible. Some patients will lose 2 to 3 kg or even more kg a week, but this is water, not fat.
He says after the first month or so, a more realistic fat loss of 1kg per week is typical on a very low kiloJoule eating plan.
“Instead of focusing on the scale, think about how loose your clothes are week to week, as quite often the scales will register muscle gain from exercise too.”

2. Fuel with Fibre
“Getting enough fibre in your diet is vital for a number of reasons, such as increased satiety, making you feel fuller for longer, as well as slowing down the digestion process, which helps to regulate blood sugar levels and avoid large peaks and troughs in insulin as well,” says Ashleigh Gale Winnett Specialist Group Dietitian.
“High fibre foods are also generally low in kiloJoules, so you can consume a higher volume without excessive kJs.”
She says fibre also promotes a healthy digestion which can improve nutrient absorption and waste elimination.
“Some types of fibre can even bind to fats and cholesterol in the digestive tract, preventing their absorption and thus reducing the number of kilojoules you actually absorb from your food”
Her top tip? If you are early on in your surgery journey, keep up your recommended fibre supplement, and try to slowly include more in your diet.

3. Protein! Protein! Protein!
Consuming sufficient protein can help preserve lean muscle mass during weight loss after surgery, which in turn can help prevent a weight plateau.
“Protein also has a higher thermic effect compared to fats and carbohydrates that can slightly increase overall energy expenditure, supporting weight loss efforts,” says Mr Winnett.
“Furthermore, protein is nutrient dense which can provide essential vitamins and minerals, especially important after surgery.”
Easy protein options are eggs, protein shakes, protein bars, lean meats, chicken and fish, tofu and high protein yoghurt.

4. Think low carb, not no carb
“When it comes to carbohydrates, aim for high fibre options; lower carb bread, beans/lentils or legumes, vegetables and a small serve of whole fruits (instead of dried or fruit juice),” says Ashleigh.
Aim to enjoy your carbohydrates from unprocessed sources that are nutrient dense and satisfying.
“Maintaining a lower carbohydrate approach assists the body by promoting the breakdown of fats for energy.
“With that being said, not all carbohydrates are created equal so don’t miss out on the variety of nutrients we get from the foods mentioned above.”
She suggests seeking ways to make your favourite carbohydrate rich foods lower carbohydrate options. For example, baked zucchini fries instead of potato chips, zucchini noodles instead of pasta, and cauliflower rice to go with your curries or stir fries.
You can try this lower carb, higher protein porridge recipe for a high fibre breakfast!
High Protein Cottage Cheese Porridge:

Ingredients:
- ¼ cup whole grain rolled oats
- 1 tsp chia seeds
- 1 tsp flaxseeds
- ½ cup unsweetened almond milk (plus extra as needed)
- 1 scoop protein powder of choice
- 1 tbsp cottage cheese
- A handful of berries
Method:
- Combine the oats, chia seeds, and flaxseeds. Add the ½ cup of almond milk and stir until well combined.
- Microwave the mixture for 1-2 minutes.
- Remove from the microwave and stir. Mix in the protein powder, adding additional almond milk if the mixture is too thick.
- Return to the microwave and cook for an additional 30 seconds to 1 minute,
- Top with a scoop of cottage cheese and a handful of berries before serving.
The amount of carbohydrates to aim for in a meal depends on what stage you’re at post-surgery. Focus on your protein targets, and remember to choose high fibre carbohydrates to aim for.
![]()
5. Dine fine!
When dining out, request a ‘to-go’ box at the start of the meal and ask for half the food to be served while the other half is refrigerated for you to take home. Ask for any sauces on the side; limit alcohol to 1-2 glasses per week; opt for oyster entrees and swap dessert for a coffee. Avoid any foods with kilojoule dense cooking methods such as fried, or sauces such as Alfredo sauce or butter sauce.
![]()
6. Plan, plan, plan
“Remember the old saying, perfect planning prevents poor performance,” says Ashleigh.
“If dining out, look at the menu before you go and be sure of what you are going to order ahead of time.”
“If you’re going to work, keep a stash of air-popped popcorn, protein shakes, protein bars and snack-sized nuts in the drawer as well as a large tub of high protein yoghurt in the fridge to get you through the week.”
“Another option is a bariatric friendly bento box with 4 to 6 of the following options: meat, devilled eggs, cheese, bell peppers with hummus, carrots with guacamole, celery and protein peanut butter and berries and nuts as options.”
![]()
7. Make mindfulness a habit
Before surgery, mindlessly inhaling half a tub of ice cream was easy to do! However, doing this after surgery can run you the risk of experiencing dumping syndrome, which can trigger nasty diarrhoea and vomiting.
“To eat mindfully, you need to eat deliberately, non-judgementally and with full attention not in front of a phone or TV,” says Georgie Beames, Winnett Specialist Group Psychologist.
“Then bring the food slowly to your lips,” says Georgie.
“Did you feel it dissolve on your tongue? Does the chewing make a sound? Is it sticky and crunchy or deliciously smooth and velvety? How warm or cold does it feel? What colour is the food and have you chewed it 20 times?”
![]()
8. Play Switcheroo
“You can fool your brain in other ways too, for instance play switcheroo with your hands. If you’re a rightie, start eating with your left hand and vice versa if you’re a leftie. Notice how much more slowly you will eat and how much extra effort it takes for you to use your knife or fork or pick up your glass of water.
“We are creatures of habit,” says Georgie.
“You might sit in the same seat each time when you give into your hunger (cravings). You can also mix up your environment by sitting in a new seat. Instead of eating out of the bag of chips, put a few in a bowl and mindfully eat them. Savour them, enjoy them and let it go and get on with your day or night.”
![]()
9. Focus on fluid
“Aim for 1.5-2L per day as a minimum with your fluids. Often if we are feeling quite hungry between meals, it may be because you’re dehydrated.
Drink fluids first, wait 30 minutes and if you still feel hunger, choose a high protein snack.”
10. Weigh minimally!
Some patients choose to weigh themselves only once a week, at the same time of day. If they encounter a stall, they should consider whether they are doing anything differently.
“However, I’m more of a fan of weighing minimally, and using other factors to track their progress,” says Winnett Psychologist Georgie Beames.
“This includes how their clothes feel. Also, non-scale victories are important, such as tracking your energy levels, your fitness levels and how you’re feeling in yourself.”
“Weighing yourself can be a big trigger for some weight loss surgery patients, and the results can send you to the fridge. If you are happy with the scales, you might give yourself a reward (such as some chocolate!), and if you are disappointed with the results, you might also feel like giving up and heading straight to the fridge.”
![]()
11. Do a little a lot – and early!
For less invasive procedures such as the Orbera Gastric Balloon and the Lap Band, gentle walking 5 to 10 minutes a day exercise can be started within 1-2 days of surgery.
For more invasive procedures such as the Gastric Sleeve or Bypass, patients should be able to sit in a chair the day of surgery and by day two or three many patients start gentle walking.
“You can start by walking just five minutes per day, then add an extra two minutes every third day,” says lifestyle consultant for the Winnett Specialist Group Sarah Pizzi.
“This can be broken up into multiple 10-minute walks. “
“Also think active v passive; walk v bus; stairs v lift; 10,000 steps v 5000 steps or 1.5 hours of walking daily.”
![]()
12. Weigh it up!
“Muscle mass is the key to helping prevent a weight plateau,” says Sarah.
“A light weight program (1-2 kg) is OK to start 10-14 days after surgery. Twice a week for 30-45 minutes is ideal. Avoid heavy weights and ask your surgeon or trainer if you are unsure. Certainly, avoid lifting children, heavy shopping, bags of kitty litter and boxes.”
She says it’s also important to avoid dynamic abdominal exercises for the first eight to 12 weeks to allow the incision to heal. Static holds such as planking are advised, and this helps to alleviate abdominal hernias near or around the incision.

13. Don’t exercise straight after eating
Always leave at least 2 hours after eating to help avoid indigestion, heartburn and getting a stitch.
![]()
14. Think “most days”
Be active on most, preferably all, days every week. Accumulate 150–300 minutes of moderate intensity or 75–150 minutes of vigorous intensity, or an equivalent combination of both, each week. Do muscle-strengthening activities on at least two or three days each week.
![]()
15. Blow up negative thoughts!
“Try dropping a mental bombshell on negative thoughts as soon as they enter your head,” says Georgie.
Instead of “I shouldn’t have had all that butter” re-evaluate the thought and come up with a more positive alternative such as “I’m going to replace butter with mustard three times a week until I get used to it.”
“When a negative thought enters your head (which will happen every day – that’s part of being a human being!), play circus music over it, or use a funny cartoon character voice such as daffy duck.”
says Georgie.
“This diffuses the power of the negative voice and it gives us a choice as to whether we want to act on that voice. Then move your attention to something else. Go for a walk around the block, have a shower, sit outside in the sun.”
Reaching a plateau on your weight loss journey is a bump in the road, not the end of it. With the right tweaks to your routine and mindset, you can get back on track. Remember, progress isn’t just about the number on the scales—it’s about how you feel, inside and out.
If you’re looking for personalised advice or need a bit more guidance, the Winnett Specialist Group is here to help. Led by Mr. Jason Winnett, our team is ready to support you through every phase of your journey.

Mr Jason Winnett
Laparoscopic and Bariatric Surgeon
P (03) 9417 1555
admin@winnettspecialistgroup.com.au
www.winnettspecialistgroup.com.au
Queens Terrace, 382 Victoria Parade, East Melbourne 3002