At Winnett Specialist Group, we are dedicated to helping you achieve long-term weight loss and better health through personalised, evidence-based care. Led by Dr Jason Winnett, a specialist bariatric surgeon with over 20 years of experience, our Melbourne-based team offers a range of weight loss procedures, including Sleeve Gastrectomy surgery. This procedure is only recommended to patients after a comprehensive medical assessment to ensure it is safe and suitable for each patient.
 Considering a Sleeve Gastrectomy?
Considering a Sleeve Gastrectomy?
If you’re considering your options or just want to understand what might be right for you, we’re here to help. We’ll start with a thorough medical assessment and talk you through whether a Sleeve Gastrectomy is the right fit. Get in touch with us here to speak with our team in Melbourne.
What is Sleeve Gastrectomy?
The Sleeve Gastrectomy is the fastest-growing weight loss surgery in the world and regarded as the gold standard bariatric procedure for most patients with uncomplicated obesity.
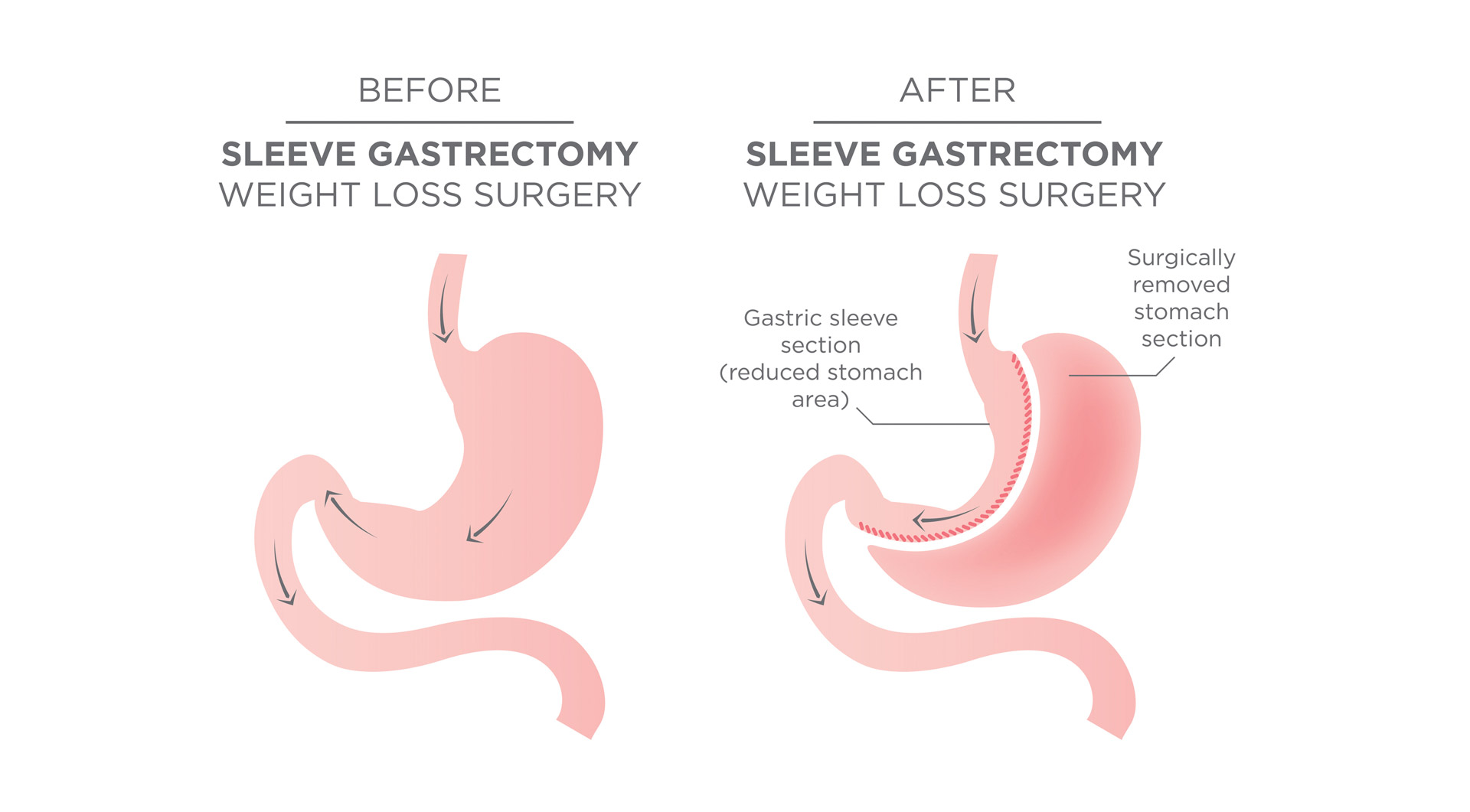
The Vertical Sleeve Gastrectomy, also called “The Gastric Sleeve” works by reducing the existing stomach to about 80% of the original stomach, leaving a smaller banana shaped stomach for food collection.
Sleeve surgery is called a “metabolic surgery” because the reduction in the stomach changes the brain’s hunger drivers, which generally makes patients feel less hungry after surgery.
The surgery is done via laparoscope and typically involves a 2-3-day hospital stay.
This surgery is regarded as less invasive than Gastric Bypass Surgery and generally involves 1-2 hours on the operating table.
Who is suitable for a Sleeve Gastrectomy?
Suitable candidates for Sleeve Gastrectomy include:
- People with a BMI >40
- People with BMI > 35 plus at least one obesity co-morbidity (for instance Type II diabetes, sleep apnoea, hypertension, lipid disorders, fatty liver disease, gastrointestinal disorders, cardiovascular disease, respiratory disease, gout, gallbladder disease and osteoarthritis).
- People who have repeatedly tried multiple diets and have failed
- Sleeve surgery can be performed on people with only mild reflux or who have insulin resistance. For people who have severe gastric reflux, or severe diabetes, the Gastric Bypass is often preferred.
- The procedure is also suitable for people who have Crohn’s Disease, or take regular anti-inflammatory medications (a bypass is more likely to result in gastric ulcers).
- There is no upper age limit, however the procedure has been found to be riskier over age 65, (although an obese but otherwise healthy 70-year-old, maybe be less risky than a 60-year-old who has multiple co-existing obesity conditions.)
- Generally, The Sleeve is the procedure of choice for the extremely obese patient (more than 180kg) as high levels of fat in the stomach do not give the surgeon much room to move, which makes the rerouting of intestines needed in a Bypass quite difficult. The Mini Bypass however may also be an option for this group, as there is less re-routing.
- People with heart disease, lung disease or transplant patients are usually better candidates for The Gastric Sleeve as it is less invasive, requires less anaesthesia and operating time.
Who is not suitable for a Sleeve Gastrectomy?
- People who are not committed to significant lifestyle change which includes healthy eating and exercise
- People who have severe reflux or severe diabetes
- People who are heavy drinkers or smokers
- People who gain weight during the surgical evaluation process
- Some mental health conditions. These include binge eating disorder, substance abuse, anxiety disorders, major depression, schizophrenia and severe bipolar, or people who have ongoing issues due to sexual abuse.
- People with these conditions may still be able to have surgery, but these conditions need to be assessed by your surgical team.
- People with esophageal dysmotility (difficulty swallowing) and gastroparesis, where food stays in the stomach, are also less suitable for sleeve surgery.
What is the treatment protocol?
- Before surgery you will be seen by our team including our bariatric physician, bariatric surgeon and anaesthetist.
- Bloods will be taken and you will also be assessed by our dietitian and fitness trainer.
- Before surgery you will go on a VLCD (very low-calorie diet), with the aim to lose 1.5k-2kg per week, 2-3 weeks before surgery.
- We use Formulite in our practice, which comes in five flavours; choc hazelnut, creamy vanilla, coffee, banana and honeycomb.
- During the procedure, the surgeon creates a narrow “sleeve” shaped like a banana, which becomes your new, smaller stomach.
- There are no large cuts, just small endoscopic incisions and you should be able to walk a few hours after surgery. The hospital stay is generally 2 to 3 days.
- After surgery you are monitored for complications, and should begin a diet of sugar-free, non-carbonated liquids for first two weeks, then progress to pureed foods for a few weeks and to regular foods a month or so after surgery.
- Every day, for life, you will be required to take multivitamins and calcium.
- You will also need to come back to rooms for regular check-ups at the two-week, six-week, three month and 12-month follow-ups.
- Those with sedentary jobs can usually return to work within 1-4 weeks, though people with vigorous jobs may need 6 weeks.
- Most people are able to drive after 3 days, but you should be off all pain medications before driving.
- Patients can shower 48 hours after surgery but cannot bathe or swim for two weeks.
- The dressings should be left on until your review by our surgical team.
What are the side effects?
- The good news is that sleeve surgery has an excellent safety profile – in fact a similar safety profile to a hip, knee or gallbladder procedure.
- Rare side effects include staple line leaks (symptoms include rapid heart rate, shortness of breath, fever and dizziness). Whilst this is a serious side effect it usually occurs in hospital and is usually very treatable.
- Other risks include blood clots, reflux, bleeding, Dumping Syndrome, and the risks associated with standard anaesthetic procedures.
- Post-surgery common side effects can include dry skin, thinning hair (which generally comes back), mood swings and body aches. Most of these symptoms settle in a few weeks or months.
- Sleeve surgery is not reversible, once the stomach is removed. However about 1 in 5 patients after 5 years may require a revision surgery. This course of action is usually considered as a last resort and has significantly more complications.
- A “re-sleeve” or conversion to bypass revision weight loss surgery is usually performed if the first sleeve fails due to a patient not adhering to diet and exercise, excess weight gain, or excess reflux.
- Whilst 1 in 5 surgeries will fail, and we do hear a lot of negative stories about weight regain in decades past, the reality is that modern weight loss procedures are highly effective for most, and Sleeve Surgery is generally regarded as a very safe surgical procedure.
- Indeed, having no treatment is a much more likely to result in one of 11-obesity-related cancers, as well as heart disease and early death.
Specialist in Sleeve Gastrectomy Surgery
Dr Jason Winnett is widely regarded as a leading specialist in bariatric surgery in Melbourne. With over 20 years of experience, he has performed hundreds of successful weight loss procedures, including the Sleeve Gastrectomy surgery, and continues to provide ongoing care and support for his patients.
His expertise includes not only primary bariatric procedures such as the Sleeve Gastrectomy, but also ongoing adjustments, band maintenance, and revision surgeries for patients experiencing complications or seeking improved results from previous procedures.

Sleeve Gastrectomy Surgery in Melbourne
Winnett Specialist Group offers Sleeve Gastrectomy surgery at several locations across Melbourne, including East Melbourne, Sydenham, Williamstown and Werribee. Our team provides personalised care for every patient, starting with a full medical assessment to ensure the Lap Band is the most suitable option.
With a strong focus on long-term outcomes, we support you through every stage of the process. This includes access to experienced dietitians, psychologists and other health professionals who work closely with you before and after surgery. Our goal is to help you achieve sustainable weight loss in a safe, supportive environment.
If you’re ready to take the next step or want to learn more, get in touch with us today by completing the form or calling us on P: (03) 9417 1555.
Frequently asked questions
- What is the safest form of weight loss surgery?
Both the Bariatric Sleeve Surgery (LSG) and Roux-en-Y Gastric Bypass (RYGB) have an equal safety record, according to a 2024 study. Both surgeries have low complication rates, and there are no deaths reported within 90 days post-surgery.
- Why is the bariatric surgery sleeve often considered safe?
The bariatric surgery sleeve removes about 70 – 80% of the stomach to create a smaller, sleeve-shaped stomach. Because it does not involve implants (like the lap band) or intestinal rerouting (like the bypass), the risks of long-term complications can be lower.
- What is the safest form of weight loss surgery for long-term results?
For long-term weight loss, both the Laparoscopic Gastric Bypass and the Laparoscopic Sleeve Gastrectomy have strong safety and success records. The safest form depends on a person’s health, weight, and conditions like diabetes or reflux. The “safest” option is the one that balances results with the potential risks and complications.
- What is the risk of complications?
Complications are rare for both surgeries. Most patients experience few issues, and the mortality rate is very low (0.03 to 2% annually), and the leakage rate is approximately 1%..
- What is the recovery time?
For Laparoscopic Sleeve Gastrectomy (LSG), the hospital stay is typically 2-3 days, with a return to routine activities in about 3 weeks. For Roux-en-Y Gastric Bypass (RYGB), recovery takes slightly longer due to the complexity of the procedure.
