What is the link between GLP-1s and suicidal ideation? What should be on a bariatric hospital discharge summary? Bariatric and Laparoscopic Surgeon Dr Jason Winnett answers GPs’ most asked questions for 2026.
Ozempic 2.0 is marked for release in 2026. How will this compare to Ozempic 1, Mounjaro, and Wegovy?
In 2026, obesity pharmacotherapy is likely to enter a phase of expanded choice.
Alongside injectable GLP-1 therapies, the pipeline now includes oral GLP-1 weight-loss agents, more potent or longer-acting injectables, and lower-frequency dosing candidates.
These advancements in weight-loss drugs, including oral medications, have been informally dubbed ‘Ozempic 2.0’.
In a study published in the New England Journal of Medicine (NEJM), involving 205 adults with overweight or obesity, daily oral semaglutide (25 mg) resulted in an average weight loss of approximately 15% at 68 weeks*1, compared with around 2% in the placebo group.
A greater proportion of treated participants achieved ≥10% weight reduction, confirming clinically meaningful efficacy for oral GLP-1 therapy (although overall weight loss remained lower than that seen with high-dose injectable formulations).
A separate NEJM study of 2,539 participants evaluated a combination strategy using cagrilintide plus semaglutide*2. At 68 weeks, mean weight loss in the combination group approached 23%, compared with approximately 16% with semaglutide alone.

However, caution remains essential.
Many therapies described as ‘2.0’ are still undergoing regulatory review and have not yet received approval from the U.S. Food and Drug Administration (FDA).
As Dr Jason Winnett emphasises, while medication innovation is welcome, it must be applied with clinical judgement, with the TGA issuing a statement in December 2025 about GLP-1 use and suicidal ideation *1b.
What is the treatment of choice for obesity in 2026?
Whilst millions around the world are embracing GLP-1 receptor agonists, compelling new evidence shows that surgery still sustains significantly greater weight loss.
A September 2025 study in JAMA Surgery (Journal of the American Medical Association) involved more than 30,458 patients tracked for two years*3.
It found that 96% of metabolic bariatric surgery patients sustained 10% of their weight loss, and 98.8% sustained at least 5%.
By comparison, 45.9% of patients on GLP-1 therapy sustained 10% weight loss, while 71.6% sustained 5% of body weight.
In the two-year follow-up, the surgical patients experienced an average of 28.3% total weight loss, compared with 10.3% in the GLP-1 patients.
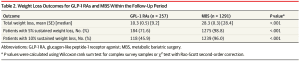
Source: JAMA, September 2025
‘Both of these treatments are game changers for patients,’ says Dr Winnett.
‘But we still need further studies to determine whether there are patient subgroups that would benefit from an earlier referral to surgery, particularly those with higher levels of obesity or people with obesity and diabetes (diabesity).’
When can patients leave hospital after bariatric surgery, and what should be on the discharge summary?
‘Most “sleeve” patients can return home after bariatric surgery in 48-72 hours and be back at a desk job within two weeks, and a more physical job in 2-6 weeks,’ says Dr Winnett.
‘Bypass patients can expect a 3-5-day hospital stay and recovery of 4-6 weeks.’
Discharge summaries can include:
- the name of the hospital or facility you were discharged from
- pathology tests
- problems/diagnoses
- clinical overview
- current medications on discharge
- any medications you are no longer taking
- allergies and adverse reactions
- discharge diagnosis
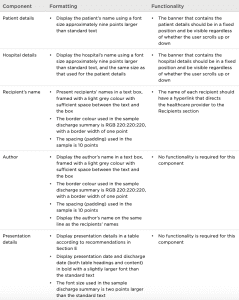
Source: Discharge Summaries from Australian Commission on Safety and Quality in Health Care
How long will my patient be on a liquid diet after bariatric surgery?
Winnett Specialist Group Dietitian Ashleigh Gale says, ‘The first day in hospital will be clear liquids in hospital, broth, juice, decaf tea or coffee, gelatine and icy poles.
‘After that, patients will be on a mostly liquid diet for 14 days, which involves limiting carbohydrates and eating mostly high-protein shakes and lump-free soups.’
When can my patient drive after bariatric surgery?
Most patients can drive a week after surgery, but Dr Winnett warns that patients should be cautioned not to drive if they don’t feel strong enough or are still on pain medications.
Please also confirm with the car insurer/broker, as driving restrictions vary between policies and may affect your cover.
When can my patient shower and play sports after bariatric surgery?
Dr Winnett says, ‘Patients can shower the day after their surgery, but having a bath and swimming should be avoided until wounds are fully healed, which can be up to 6 weeks after surgery.’
A systematic review published in Obesity Surgery, which analysed outcomes from thousands of post-surgical patients, found that those who engaged in regular exercise after surgery achieved an additional 4.2% reduction in BMI*4 compared with patients who remained inactive.
‘GPs should encourage gentle walking and gentle weights, but discourage competitive sport for the first few months, especially if there is risk of stomach injury.’
What vitamin deficiencies are most likely after bariatric surgery?
‘GPs should consider post-operative 6-monthly and 12-monthly screening for iron, Vitamin B12 and folic acid,’ says Dr Winnett.
‘Opt for 3-monthly screening for Vitamin D, Vitamin A, Vitamin E, and thiamine (if there is persistent vomiting) or copper if there are unresolved iron issues.’
How much weight can patients expect to lose after bariatric surgery?
In the short term, most weight loss occurs in the first 6-9 months post-surgery. Generally, weight loss will continue for 12 months and then stabilise.
‘A patient of 150kg may typically expect to lose about 10 to 15kg in the first month after surgery,’ says Dr Winnett.
‘One thing I’ve noticed with many patients is that this initial weight loss can be rapid and can sometimes give patients an unrealistic sense of how much weight loss is possible, because a lot of the initial loss is water – not fat.’
That’s why it’s vital that these expectations are managed in primary care, particularly after three months, when patients are less likely to see their surgeon.
‘After the first month or so, a more realistic fat loss of 1-2 kg per week is typical on a very low-kilojoule eating plan,’ says Dr Winnett.
How should GPs help patients navigate ‘dumping syndrome’ after bariatric surgery?
Dumping syndrome occurs when high-sugar and high-energy foods (think soft drinks, fruit juices, white bread, pasta, and rice) move too quickly from the stomach into the small bowel.
‘There are two types of dumping: early dumping, which occurs 1 to 30 minutes after eating*6, and symptoms include fatigue, sweating, hypotension, nausea, diarrhoea and sweating. Then there’s later dumping syndrome, which occurs 1-3 hours after a meal and is an incretin-driven hyperinsulinaemic response.’
This can lead to reactive hypoglycaemia, presenting with adrenergic and neuroglycopenic symptoms including sweating, anxiety, fatigue, tremor, hunger, and confusion.
‘The best way to avoid dumping syndrome is to simply encourage patients to change their diet after surgery,’ says Dr Winnett.
This change of diet includes:
– Avoiding liquids for 30 minutes after a solid food meal
– Avoiding sugar, carbohydrates, and junk food
– Avoiding greasy or spicy foods
– Avoiding large meals (regardless of food type)
– Eating smaller portions more often, choosing foods that are low in kilojoules
– Avoiding alcohol
– Opting for a high-fibre diet of unprocessed carbohydrates and low glycaemic index foods, which can stabilise blood glucose fluctuation that occurs with late dumping syndrome
– Taking alpha-glucosidase inhibitors, which can help delay the digestion of carbohydrates (speak to a healthcare professional before taking this medication)
Looking ahead: supporting your patients in 2026
For GPs helping patients navigate weight loss, success lies in knowing when to prescribe, when to refer, and how to support patients through their post-operative journey with vigilant monitoring and dietary guidance.
Whether your patient chooses medication or surgery, the goal remains the same: sustainable, healthy weight loss with proper medical oversight. Stay informed, stay engaged, and don’t hesitate to collaborate with bariatric specialists to ensure the best outcomes for your patients.
For more information on bariatric surgery or to discuss patient referrals, contact Dr Jason Winnett and the team at Winnett Specialist Group.
P (03) 9417 1555
admin@winnettspecialistgroup.com.au
www.winnettspecialistgroup.com.au
Queens Terrace, 382 Victoria Parade, East Melbourne 3002
Sources
1. Oral Semaglutide at a Dose of 25 mg in Adults with Overweight or Obesity;
1b.TGA GLP-1 Warnings about suicidal behavior
2. Coadministered Cagrilintide and Semaglutide in Adults with Overweight or Obesity
3. Obesity Treatment With Bariatric Surgery vs GLP-1 Receptor Agonists
4. Exercise Following Bariatric Surgery: Systematic Review