
With Dr Jason Winnett, bariatric and laparoscopic surgeon
A recent analysis of the comparative efficacy and cost-effectiveness of GLP-1 receptor agonists versus metabolic bariatric surgery (MBS) provides compelling evidence that surgery still sustains significantly greater weight loss*1.
Efficacy of metabolic bariatric surgery vs GLP-1 agonists
The September 2025 study in JAMA (Journal of the American Medical Association) Surgery1 involved more than 30,458 patients. It found that after two years, 98.8% of surgical patients maintained at least a 5% reduction in their starting body weight, and 96% sustained a weight loss of 10% or more of their starting weight.
By comparison, among those using GLP-1 agonists, 71.6% maintained at least a 5% weight loss, and 45.9% achieved and sustained a 10% reduction.
The difference in total weight loss was also striking: after about two years, the surgical patients had lost an average of 28.3% of their starting body weight, while those treated with GLP-1s lost an average of 10.3%.
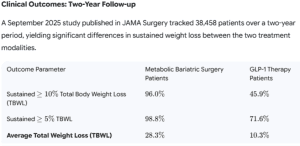
Source: JAMA, September 2025
Melbourne-based bariatric and laparoscopic surgeon Dr Jason Winnett says, ‘This latest dataset indicates that MBS provides a significantly more robust and durable reduction in body mass than pharmacotherapy.’
Comparing cost-effectiveness for patients: surgery vs GLP-1s
Dr Winnett concurs with the authors’ conclusion that surgical treatment may offer ‘greater effectiveness at a lower cost’ than obesity management medication for the durable treatment of obesity.
The JAMA study also found that patients who had weight-loss surgery spent around US$11,869 USD (about AU$18,330) less on treatment compared with those using GLP-1 medications.
Despite the upfront costs of surgical treatment being higher at the beginning of the weight-loss journey, the ongoing expense of weight-loss medications quickly adds up. Over the two-year period, surgery not only delivered greater weight loss, but also ended up being more cost-effective.
‘Both of these treatments are game changers for patients,’ says Dr Winnett. ‘But we still need further studies to determine whether there are patient subgroups that would benefit from an earlier referral to surgery, particularly those with higher levels of obesity or people with obesity and diabetes (diabesity).’
Financial burden of GLP-1 therapy for patients
According to the American JAMA study, weight-loss medications tend to cost around US$37,000 (approx. AU$56,990) over a two-year period. How does this compare in Australia, where medications are significantly cheaper?
Semaglutide
In Australia, at a large chemist chain, semaglutide for weight loss currently costs about $250 per month at lower doses (.25mg and 0.5mg), or $6000 over two years.
At the higher doses (2.7mg) patients could expect to pay about $370 per month, or about $8800 over two years, with slight variations depending on the pharmacy of purchase.
Tirzepatide
Tirzepatide (Mounjaro), which was recently found to be slightly more effective than semaglutide (Ozempic and Wegovy) in a head-to-head study, also has a considerable monthly outlay.
Tirzepatide here in Australia is roughly $280 per month for a starting dose of 2.5mg or $690 per month for the highest dose.
Over two years, this would equate to $9,360 for a low dose or $16,800 for the high dose, again with slight variations depending on where it was purchased.
So, should patients be encouraged to opt for weight-loss surgery or GLP-1s?
Dr Winnett says that for patients who do not want these large ongoing monthly costs, or who are severely overweight, surgery remains the optimal option for cost and effectiveness.
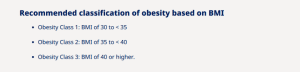
‘On the other hand, people with Class 1 obesity who often have only 5 or 10kg to lose may prefer the ongoing costs of GLP-1s. They can then try to taper 6 or 12 months after weight is stable, when exercise, sleep, and healthy eating habits are entrenched.
‘Although large studies show that for most GLP-1 patients, at least half the lost weight simply piles right back on*2 when they cease treatment, other studies show slow tapering of 2.5mg of semaglutide*3 can be successful.’
GLP-1 weight-loss medications: pros and cons
Weight loss is not the only upside of GLP-1s, according to a landmark 2024 New England Journal of Medicine study*4.
Among the 3,533 participants with Type II diabetes, a three-year follow-up showed that those taking semaglutide had a 24% lower risk of a primary kidney event and an 18% lower risk of a major cardiovascular event.
‘But there are side effects, and the treatment of obesity is not like taking paracetamol to treat a cold, or an infection where you take antibiotics and you’re done,’ says Dr Winnett.
‘Obesity is a chronic disease, just like high blood pressure and diabetes. The patients who fare best are those who reach out early to their care team for help. Some people may need to stay on GLP-s long-term.
‘And for people with “diabesity” or more complex or severe obesity, assessing the medical benefits of metabolic surgery early on is vitally important.’
Surgery vs GLP-1s: adverse effects and safety considerations
GLP-1s
The most common side effects of GLP-1 class receptor agonists include nausea, stomach pain, diarrhoea and constipation.
Very rare side effects such as gastroparesis or failure of the stomach to empty are usually resolvable, but of the millions who take GLP-1s, there are currently 2089 US lawsuits in October 2025. At the time of this article’s publication, no settlements have been reached.
Bariatric surgery
Risks for bariatric surgery are extremely low compared to previous decades.
‘Today, a bariatric surgery procedure has a similar safety profile to any other standard operation like a knee or hip replacement,’ says Dr Winnett.
The current Bariatric Surgery Register 2024 shows that since the registry started, there has been a total mortality rate of 70 per 178,000 bariatric surgeries in Australia*5.
‘The risk of NOT having bariatric surgery for severely obese people means a much greater risk of premature death,’ says Dr Winnett. ‘This is especially in younger people (20-39 age group), where research shows that years of life lost (YLL) due to obesity are 8-10 years on average.*6
Tips for follow-up after GLP-1 discontinuation
For patients who opt for GLP-1 treatment, ongoing monitoring is essential to support positive long-term outcomes.
‘It’s a good idea for GPs to follow up within 1 month of stopping medication or if the weight gain is more than two or three kilograms,’ says Dr Winnett. ‘Regular contact helps patients feel supported and allows early intervention if weight starts to increase.’
He recommends patients use the new Body Roundness Index to measure their body and urges doctors to continue verbally encouraging patients even when the scale doesn’t move in the desired direction.
‘Remind patients that some rebound is not a failure; rather, it is a normal part of chronic disease management.’
Recommended preoperative assessments for bariatric surgery candidates
Investigations for bariatric patients should include:
- Routine labs: (fasting lipids, full blood count, urea and electrolytes, liver function tests, coagulation screen, urinalysis, fasting glucose and glycated haemoglobin (HbA1c) to screen for diabetes)
- C-peptide level to predict diabetes remission
- Nutritional screen: iron studies, vitamin B12 folate 25-OH, vitamin D
- Gastrointestinal evaluations, such as abdominal ultrasound and endoscopy may be required.
- Electrocardiogram and polysomnography may be required if cardiovascular or sleep apnoea is suspected.
- Psychiatric evaluation and psychiatry referral if known or suspected psychiatric illness or substance abuse.
While today there are no absolute contraindications to bariatric surgery, relative contraindications for the more extensive surgeries, such as sleeve and bypass, do exist, including heart failure, unstable coronary artery disease, end-stage lung disease, drug and alcohol dependency, impaired intellectual capacity and Crohn’s Disease (for BYPASS).
Bariatric surgery with the Winnett Specialist Group
A few important considerations can help optimise outcomes and support patients through every stage of their bariatric journey.
- 30 years of data show us that surgery outcomes have significantly improved, including a low morbidity and mortality annually (about 0.03 to 2% annually) in a cohort of patients that most certainly face premature death.
- Procedures used to take 2-4 hours; now, many procedures are much shorter.
- At the Winnett Specialist Group, patients are seen by both Dr Winnett and dieticians twice pre-operatively, as well as by specific specialists such as cardiologists, respiratory physicians, endocrinologists, clinical psychologists, and/or psychiatrists, as required.
- All patients receive dietetic and psychological support at the Winnett Specialist Group throughout their weight loss journey.
- Follow-up with the Winnett Specialist group surgery is 3-monthly and lifelong.
Supporting patients’ weight-loss journeys
While both GLP-1 medications and surgery can be effective for weight loss, the evidence continues to show that metabolic surgery delivers greater, longer-lasting results, and often at a lower overall cost.
While surgery is the more effective and durable option, GLP-1s provide a valuable alternative for those seeking a non-surgical approach.
As Dr Winnett emphasises, patients benefit most when clinicians provide individualised guidance to help determine the most appropriate treatment pathway based on medical, psychological, and lifestyle factors.
‘Health professionals are not only helpers on the weight loss journey, but importantly, they’re also listeners to help patients and answer questions.’
If you have patients considering bariatric surgery, contact the Winnett Specialist Group for expert, evidence-based care and ongoing support.
P (03) 9417 1555 admin@winnettspecialistgroup.com.au
www.winnettspecialistgroup.com.au
Queens Terrace, 382 Victoria Parade, East Melbourne 3002
Sources
1 Obesity Treatment with Bariatric Surgery vs GLP-1 Receptor Agonists
2 Weight gain after stopping new obesity drugs, Science alert
4 Effects of Semaglutide on Chronic Kidney Disease in Patients with Type 2 Diabetes
5 Bariatric Surgery Registry Report, 2024



