
Medication vs surgery – lowest surgeries on record in 8 years
“In recent times, we have seen a huge shift in the weight loss zeitgeist – as more Australian patients opt for a pharmaceutical approach with drugs such as Semaglutide,” says Melbourne Bariatric and Laparoscopic Surgeon Mr Jason Winnett.
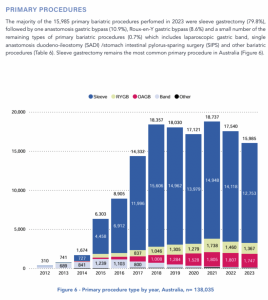
The recently released 2023/2024 Australian and New Zealand Bariatric Surgery Registry’s Annual_Report_Summary, shows an 8 year-low for bariatric surgeries – with 15,985 surgeries performed in 2023/24, compared to 17,540 in 2022 and 18,737 in 2018.
“With multiple interest rate increases, people have faced the significant cost of living challenges, and many are taking the view of trying a less-invasive ‘pharmaceutical-first’ approach with new line medications such as Semaglutide (Wegovy® and Ozempic®),” he says.
“Even though surgery will be cheaper in the long run after the first two years, many patients enjoy the minimally invasive nature of the medication, have fewer side effects and experience results that approach the efficacy of surgery,” he says.
However, he says that surgery is still the gold standard for obese patients because – unlike medications where the weight usually returns when you stop – this is far less likely to happen even 4-years post-surgery, as the 2023/2024 Bariatric Surgery Registry outcomes vindicate.
“We can still confidently say that today bariatric surgery has an excellent efficacy, as well as a good morbidity and mortality profile, with a risk profile similar to knee replacement or appendectomy,” says Mr Winnett. Since the Bariatric Surgery Registry started tracking surgeries in Australia more than a decade ago, surgeons have performed 179, 690 surgeries with a total of 62 deaths recorded within 90 days of surgery (0.03% risk). “Of course, adverse events and mortality are very important. But this, almost negligible risk, needs to be weighed up against patients almost certainly living a life of severe disability or dying prematurely from a co-morbidity such as heart disease or sleep apnoea if they don’t have the surgery at all.”
He says there is little doubt that for very obese patients, surgery is still the gold standard. Around 70% of patients no longer need insulin for diabetes one year after surgery, and average weight loss across all bariatric procedures continues to be nearly a third of total weight even after year 4 post-surgery.
But he says that an increasingly large subset of patients may find other strategies more appealing than surgery. Pharmaceutical approaches work well for people looking to lose 10 to 20kg. And although the weight usually returns after they stop the medication, many just see this as a medicine they take for the rest of their lives, as they would for cholesterol, blood pressure or depression.” He says that there is also evidence in a 2024 Journal of the American Medical Association cohort study, which shows that patients who take Glucagon-like Peptide Receptor Agonists (GLP-1), such as Semaglutide, have a reduced risk of 13 different cancers.
“This study of more than 1.6 million patients with type 2 diabetes (T2D) who had no prior diagnosis of 13 obesity-associated cancers found that patients with T2D treated with GLP-1RAs vs insulin had a significant risk reduction in 10 of 13 of these cancers, including oesophageal, colorectal, endometrial, gallbladder, kidney, liver, ovarian, and pancreatic cancer as well as meningioma and multiple myeloma. No decrease in cancer risk was associated with GLP-1RAs compared with metformin.”
However, he says that conflicting research on weight loss medications is even more reason for patients to undertake long-term weight loss programs under the care of a GP or weight loss specialist. “At the same time, we are also seeing conflicting evidence that has come out of the San Antonio breast conference this month, which shows whilst GLP-1s may be protective after cancer treatments, they may actually make recurrence of hard-to-treat cancers such as triple negative cancer much more resistant to chemotherapy – when taken before cancer treatment.”
Mr Winnett says the intricacies involved in treating patients with co-existing health conditions made it even more important for them to be wary of the options available for weight loss – and their side effect profiles.
“Right now, there’s certainly a high degree of uncertainty for what GLP-1s means in terms of bariatric surgery volume in the long term. But for patients and doctors alike, with all the different treatment options that now exist, we truly are entering a golden age. The challenge for the next few years is making sure patients are able to access the drugs they need and that patients continue to work with their GPs and specialists on their weight loss journey rather than try to do it alone,” he says.
The rise of the ‘mini-surgeries’
Recent 2022 revisions to BMI guidelines now allow more patients in Australia to meet eligibility criteria for life-changing bariatric surgery than ever before.
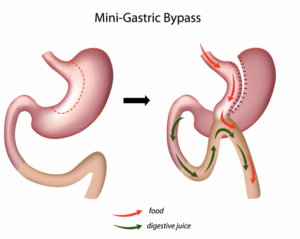
While Gastric Sleeve surgery (or Sleeve Gastrectomy) is still the ‘go-to surgery’ for uncomplicated obesity and pre-diabetes, the mini-gastric bypass takes about 50 minutes less time on the table, so the anaesthetic risks and complications are lower than standard bypass surgery, says Mr Winnett.
“With the miniature procedure, there is only a single anastomosis, and the surgeon reroutes just one portion which is longer and even lower down the small intestine, bypassing 20% of the digestive system,” he says.
Mr Winnett includes that the Mini Gastric Bypass has more complications than the Gastric Sleeve surgery, but fewer than the standard Gastric Bypass. In the 2023/24 year of surgical data, Sleeve Surgery ranked as Australia’s most popular surgery, however, the mini-bypass has overtaken the Roux-en-Y gastric bypass as the second most popular procedure.
What about inflatable options? “For the increasing numbers of Class 1 patients, we are seeing some new options to the standard sleeve gastrectomy,” says Mr Winnett.
“The Orbera Intra Gastric Balloon for instance is recommended for patients with a BMI of 27kg/m2 or above. This is generally recommended for Class X patients who wish to lose a small amount of weight, such as 10–15 kg It tends to be popular after pregnancy weight gain.”
He says the procedure involves an inflatable silicone balloon being placed in the stomach endoscopically in a twilight sedation procedure. The procedure generally takes around 20 minutes. “After 6-12 months, the balloon is removed, and although weight loss is quite variable, some patients have used it before as a definitive surgery to reduce liver volume, and some women particularly have found it useful to lose the extra 10–15 kg gained post pregnancy. When the balloon is removed, usually only a few kilograms come back.”
GP investigations before any bariatric surgery or weight loss medications? include
- Routine labs – fasting lipids, full blood count, urea and electrolytes, liver function tests, coagulation screen, urinalysis, fasting glucose and glycated haemoglobin (HbA1c) to screen for diabetes)
- C-peptide level to predict diabetes remission
- Nutritional screen – iron studies, vitamin B12 folate 25-OH, vitamin D
- Gastrointestinal evaluations such as abdominal ultrasound and endoscopy may be required.
- Electrocardiogram and polysomnography may be required if cardiovascular or sleep apnoea is suspected.
- Psychiatric evaluation and psychiatry referral if known or suspected psychiatric illness or substance abuse.
While there are no absolute contraindications to bariatric surgery today, relative contraindications for the more extensive surgeries such as sleeve and bypass do exist – including heart failure, unstable coronary artery disease, end-stage lung disease, drug and alcohol dependency, impaired intellectual capacity and Crohn’s Disease (for BYPASS).
Points to remember
- Surgery outcomes have significantly improved based on 30 years of data and low morbidity and mortality annually (about 0.03 to 2% annually) in a cohort of patients that most certainly face premature death.
- Procedures used to take 2-4 hours – now they are much shorter for many surgeries.
- At the Winnett Specialist Group, patients are seen by both myself and our dieticians twice pre-operatively, as well as specific specialists such as cardiologists, respiratory physicians, endocrinologists, clinical psychologists and/or psychiatrists as required.
- All patients will receive dietetic and psychological support throughout their weight loss journey at the Winnett Specialist Group.
- Follow-up with Winnett Specialist group surgery is 3 monthly and lifelong.
Winnett Specialist Group takes a holistic approach to weight loss. We believe in offering patients a full spectrum of support through a multi-disciplinary team, comprising a weight loss surgeon, specialist physicians, dietitian, exercise physiologist and psychologist who are all involved in the patient’s journey, not just at the time of surgery but in the months and years that follow. For more information please contact us or call (03) 9417 1555.

Mr Jason Winnett
Laparoscopic and Bariatric Surgeon
P (03) 9417 1555 admin@winnettspecialistgroup.com.au
www.winnettspecialistgroup.com.au
Queens Terrace, 382 Victoria Parade, East Melbourne 3002
Sources:
- 2023_BSR_Annual_Report_Summary.pdfBariatric surgery is as safe as other common operations: an analysis of the ACS-NSQIP – Surgery for Obesity and Related Diseases, 2024 GP-Based weight loss program can reverse Type2 diabetes, BMJ 2017
Arthritis Australia 2018 Obesity Epidemic in Australia Report
Weight loss and blood pressure control, Hypertension Journal.
Modest weight loss reduces breast cancer risk, Asco Post, 2018
Weight Loss Improves Mood In Depressed People, New Research Shows | ScienceDaily 2009
More obese people in the world than underweight, says study – BBC News
National Cancer Institute, Obesity and Cancer, 2017
Criteria for bariatric surgery ANZMOSS
Re-examining the Link between Obesity and Wages | St. Louis Fed



