
The specialists at Winnett Specialist Group offer GPs their top tips on how to help patients deal with ‘food noise’ (intrusive food thoughts).
The Surgeon’s Perspective
“In the tight time restraints of a GP weight loss consult, it’s often difficult to take a waist circumference measurement, let alone evaluate the intrusiveness of a patient’s food cravings,” says Mr Jason Winnett, bariatric and laparoscopic surgeon at the Winnett Specialist Group.
According to one RACGP study in regional Victoria*1, lack of time, lack of effective options and appropriate language, and concurrent mental health issues were all concerns for GPs when having the weight conversation with patients. Comments from GPs included:
“It is an enormous mental health issue…it’s what is going on in the mind that is the most important bit.”
“If somebody’s a bit um, if they’re fragile, you certainly wouldn’t be bringing up their weight.”
Mr Winnett says that just like suicidal thoughts or rumination over a past lover, food thoughts can be extreme, long-term, and can often cause significant dysfunction. “Some patients will tell me they spend hours a day thinking about food. So a brief question to help patients understand whether they are eating out of physical or emotional hunger, and how intrusive their food thoughts are (including feelings related to shame and anxiety about their weight), is often a very helpful step in the right direction.”
He says “food noise” is a popular term for polyphagia, or extreme hunger, which can often be caused by diabetes, premenstrual syndrome (PMS), hyperthyroidism, atypical depression and anxiety disorders, and less commonly with conditions such as Prader-Willi Syndrome.
His top tips for managing cravings and weight loss in GP practice include:
- ASKING for permission to discuss weight. “Always address any other chief medical concerns first; never make weight the main focus of the consult unless that’s what they came for.”
- ASSESSING risks and causes of obesity (e.g., family history, lifestyle, underlying medical conditions). Also, always weigh up any co-existing depression and use of antidepressants or antipsychotic medications. One JAMA meta-analysis of 58,000 patients found that obese patients have a 55% increased risk of becoming depressed in their lifetime compared to non-obese patients*2.
- ADVISING on treatment options. Psychological support may be enough for some, but for those with a BMI of 30 or more, medical and surgical interventions may be necessary, especially if there are comorbidities.
- AGREEING on two or three measurable prescriptive goals.
- ASSISTING in accessing psychologists, bariatric surgeons, and weight loss medication.
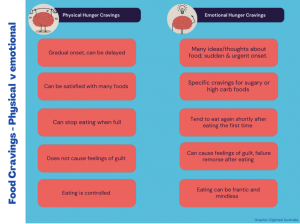
Teaching patients the difference between physical hunger and emotional hunger is important.
Obesity Medications
To what extent do obesity medications reduce polyphagia?
“For people with diabetes and obesity, quite often medications such as Semaglutide can quieten cravings, and patients often tell me that the urge to constantly think about food wanes significantly. We see a similar effect with Sleeve surgery, Bypass surgery and to a lesser degree, the intragastric balloon.”
He says the potency of Semaglutide was first confirmed in 2021 in The New England Journal of Medicine, resulting in 14.9% weight loss compared to 2.4% placebo in 1961 subjects over 68 weeks.*3
However, he counters that the cost of monthly medication and the fact that patients generally regain weight again when they stop medications*4 are important considerations for GPs.
“Side effects commonly include diarrhoea and nausea and rarely pancreatic inflammation.”
“A very rare side effect is gastroparesis*5, a permanently paralysing condition which prevents proper stomach emptying and can cause vomiting, a feeling of fullness, pain and bloating.”
“It is a condition which is chronic and while can be managed cannot be cured.” Mr Winnett says weight loss medications have an important place for the treatment of diabetes and extreme obesity and are also important for pre-bariatric surgical patients. “However, given current supply issues globally and side effect profile, it should be prescribed “judiciously”.”
Psychological Interventions
“With the Internet, TV, Twitter, Tik Tok, and home delivery Apps at our fingertips, we are living in an era where we are constantly surrounded by food 24/7,” says Winnett Specialist Group Psychologist Georgie Beames.
Georgie specialises in emotional eating and weight loss using somatic stimulation techniques and cognitive therapy as well as EMDR (Eye Movement Desensitisation and Reprocessing) which has been used for many years in the treatment of addiction and trauma patients.
“Sometimes the level of food chatter we have in our head can have very deep roots,” she says. “It may be linked back to childhood if there were frequent comments about weight and food portions. Or at the other end of the scale, there were very few boundaries set when it came to eating healthy food.”
Top Tips for GPs:
- When patients experience intrusive thoughts, often triggered by stress, anger, sadness or boredom, encourage them to pause before going to the fridge.
- Mindfulness, exercising, or painting their nails so they can’t touch food for at least 10 minutes until a craving passes are good distraction techniques.
- A 5-minute body scan process of box breathing (breathe in for 4, hold for 4, out for 4) can also help stave off a craving and help patients to take themselves off automatic food pilot.
- Tell patients that medication or surgery can make the journey easier, but ultimately the patient needs to accept that they ultimately decide to get on the treadmill or what to put in their fridge.
- Encourage changing seats to the one they are sitting in if they experience a sudden craving.
- Encourage patients to weigh themselves only once a week, not every day.
- Encourage patients to avoid junk food in the house.
- If patients do want to keep ice-cream or chocolate as a small treat, they can hide it in the back of the freezer or pantry. Out of mind, out of sight!
The Dietitian’s Advice
The mainstay of dietary requirements for weight loss is eating protein at EVERY meal, says Winnett Specialist Group Dietitian Ashleigh Gale.
“This includes eggs, lean meats, chicken and fish, tofu, yoghurt (encourage patients to seek out high protein brands in supermarkets that have 17g or more of protein on the label),” Her other top tips include:
- Substitutes – Substitute rice, pasta, and white or brown bread with lower carb bread, beans/lentils or legumes, and smaller amounts of pumpkin or potato.
- Portion Control – Think smaller portion size when eating. Use a dessert plate instead of a dinner plate.
- Plate Composition – Fill the plate with protein first as well as bulking out your portion and leafy salads or veggies, rather than white bread or pasta or potato salads.
- Dressings –Choose lemon vinaigrette with small amounts of extra virgin olive oil rather than any creamy dressings.
- Low GI Fruits – Eat low GI fruits such as apples, oranges, strawberries, blueberries, and plums as opposed to sweets or high GI fruits such as ripe bananas, rockmelon, pineapple, and watermelon.
- Healthy Snacks – Good options for savoury cravings include nuts, turkey breast instead of salami, fresh peeled prawns, and grilled seafood instead of sausages and cured meats.
- Drink Control – Downsize glasses at home. Opt for a small (125 ml) wine glass rather than a large (250 ml) glass. Drink only water, do not buy or consume juices and soft drinks. Limit to one or two glasses of alcohol a week only – especially for bariatric surgery patients.
- Exercise and Sleep – Aim for at least 10,000 steps a day plus at least two or three resistance sessions a week. Make sleep a priority.
Remember, addressing food noise and weight management requires empathy, respect, and a focus on overall health. If you have any questions or would like to discuss this further, feel free to contact our team at Winnett Specialist Group. Let’s continue working together to provide the best care possible for our patients.
Mr Jason Winnett
Laparoscopic and Bariatric Surgeon

Georgie Beames
Psychologist

Ashleigh Gale
Dietitian
www.winnettspecialistgroup.com.au
Queens Terrace, 382 Victoria Parade, East Melbourne 3002
References:
5 The weight-loss drug Wegovy may also help treat addiction (sciencenews.org)
7 Ozempic Lawsuit: May 2024 Gastroparesis Lawsuit Update (drugwatch.com)




