Does metabolism really slow with age – and by how much? How does the mini-gastric bypass help metabolic profile? Melbourne bariatric and laparoscopic surgeon Mr Jason Winnett separates metabolism and weight loss facts from the myths.
What causes a slow metabolism anyhow?
“In reality, it is only patients with underlying metabolic disorders such as hypothyroidism, Cushing Syndrome or low testosterone that fit the definition of a “slow” metabolism,” says Mr Winnett.
In these cases, patients are best served by addressing the underlying hormone problem with a GP or weight loss specialist who can identify the issue with blood tests, and help treat it with lifestyle changes, medication and/or surgery if required.
For the vast majority of overweight people, who don’t have an underlying metabolic medical issue like this though, there is currently little solid scientific research that weight gain is linked to a slow metabolism.*1
In fact, patients with obesity often have faster metabolisms, according to the Cleveland Clinic. *2 This is because their bodies need more energy to keep basic body functions going.
“So, if you’re thinking that you need to ‘reset a slow metabolism’ with fad diets, a juice detox or drinking lots of coffee and eating chillies, you’re probably on shaky scientific ground. There is no evidence that any of these things will make more than a small or negligible difference to people who are seriously overweight.”
What about the notion that our metabolism slows down with age?
Recent research reported in Harvard Health*3 involving more than 6400 people in 24 countries has debunked the idea that our metabolism slows down in middle age. At least, by as much as was commonly thought.
In fact, metabolism remains rock-solid right up until the age of 60, and then it declines steadily, reaching a level 26% lower than mid-life by the age of 90, as found in the study.
Does extreme diet and exercise change your metabolism?
While regular weightlifting can improve muscle mass, extreme exercise and extreme diet does the opposite. As clinical research on 14 biggest loser contestants *4 found, these contestants put on their original weight, or more, years after their time on the show where they exercised for hours each day and consumed very minimal kiloJoules.
“The reason why the biggest loser contestants struggled to lose weight long-term is because the body has a built in system to defend its highest weight “set point”, says Mr Winnett.
If we use the analogy of holding your breath – after a couple of minutes of trying to stop breathing, your body will simply force you to breathe again. It’s the same with weight and set point.
In fact research finds that diet changes alone will fail in 80% of obese people according to a recent meta-analysis of 29 long-term weight loss studies.*5
“The set point is the body’s way of responding to the threat of famine. This is also why weight loss is so very hard, the bigger you are and the longer you have been overweight,” says Mr Winnett.
He says medically supervised weight loss programs can help somewhat and a study of 10,000+ patients showed up to 5.8% body weight loss on average after five years, in a study of 2,777 patients. *6.
“But this is not enough for everyone. While it’s doable to lose 5, 10kg, or 15kg, especially when the brain hunger drivers are not so strong, in the severely obese, the hormones driving your hunger are working hard against your set point and may require interventions such as medications or surgery. For someone weighing 70kg, a 5.8% weight loss is a meaningful 4 kg. However, for someone who weighs 180 kg, a 5.8% drop in body weight (equivalent to 10.44 kg) just won’t be enough.”
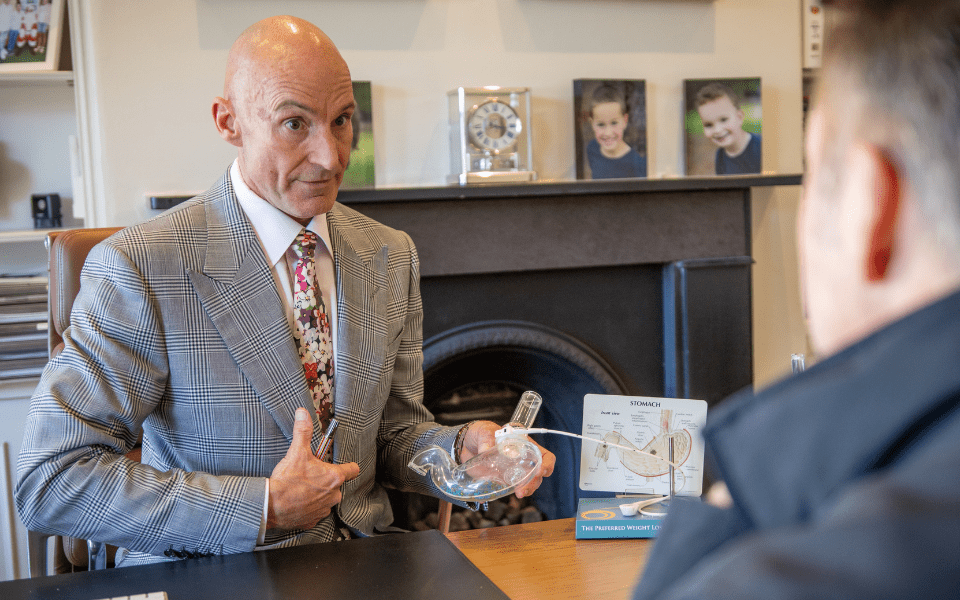
What is the Mini Gastric Bypass and how can it help reset metabolism and resolve diabetes?
Some studies show that while dietary changes do not change metabolism, bariatric surgery can *7 – by reducing branch chain amino acids, which are known to be associated with insulin resistance.
So just how does the Mini Gastric bypass work and how can it help with improving metabolism and diabetes? Just as the Laparoscopic Sleeve and regular Bypass surgeries have metabolic effects, similarly the Mini Gastric Bypass does too. Additionally, it is a good option for people looking to put diabetes into remission.
What is the difference between procedures?
The Mini-Gastric Bypass procedure is a simpler procedure than the Roux-en-Y-Gastric bypass; takes about 50 minutes less time on the table and so the anaesthetic risks and complications are lower.
During the standard Gastric Bypass, the stomach is made much smaller and shaped into an egg-sized pouch that holds about 150mls of food. The small intestine is then split into two pieces known as a double anastomosis (or two surgically made channels that connect organs).
The surgeon attaches one anastomosis to the bottom of the new pouch. The second is rerouted lower down to the small intestine, bypassing most of the digestive system and small intestine.
With the miniature procedure, (single anastomosis), the pouch still holds about 150ml of food, and the surgeon reroutes just one portion which is longer, even lower down the small intestine. This bypasses 20% of the digestive system.
Mr Winnett says that the Gastric Sleeve surgery has the lowest complications rate (1.3%), so it is the “go to” surgery for people without diabetes. However, according to Bariatric Surgical Registry Report for 2022 *8 for the increasing numbers of obese people with diabetes, the Mini Gastric Bypass has a complication rate of only 3.7% compared with 5.3% for the Gastric Bypass.
The Mini Gastric Bypass is now also clinically proven to have better long-term diabetes remission without medication than the Sleeve *9
What else can I do?
- Exercise for muscle gain – muscle burns more kJs than fat.
- Eat protein to increase muscle mass. Protein requires your body to use more energy to digest.
- Avoid white carbs (pasta, rice, cakes, biscuits). However, carbs from leafy greens, legumes and beans are ideal because the glycaemic load is small and fibre load high to help keep insulin stable.
- If you’re not having surgery, try intermittent fasting under doctor supervision. Many studies in fact now show that fasting is a good diet strategy overall and improves biomarkers of disease such as diabetes and obesity*10.
- However, if you’ve had surgery, intermittent fasting is NOT recommended for the first three months, says Mr Winnett.
If you find yourself navigating the complexities of metabolism, weight loss, or considering surgical options, don’t hesitate to reach out. Contact the Winnett Specialist Group and book a consultation with Mr. Jason Winnett for personalised guidance towards achieving your health goals.

Mr Jason Winnett
Laparoscopic and Bariatric Surgeon
P (03) 9417 1555
admin@winnettspecialistgroup.com.au
www.winnettspecialistgroup.com.au
Medical References:
Mayo Clinic Metabolism and Weight Loss; How you burn calories, November 2022 *1
Cleveland Clinic Metabolism Overview *2
Surprising findings about metabolism and age – Harvard Health *3
Persistent metabolic adaptation 6 years after “The Biggest Loser” competition – PubMed (nih.gov) *4
Maintenance of lost weight and long-term management of obesity – PMC (nih.gov) 5*
Gastric surgery changes metabolism: study › News in Science (ABC Science) *7
Bariatric-Services-Registry-Annual-Report-2022 (monash.edu) *8
Intermittent fasting: the science of going without – PMC (nih.gov) *10