
GPs play a crucial role in the management of obesity and recent 2022 revisions to BMI guidelines now allow more patients in Australia to meet eligibility criteria for life-changing bariatric surgery than ever before.
Laparoscopic and bariatric surgeon Mr Jason Winnett offers the pros and cons, from the least complex surgery to the most complex.
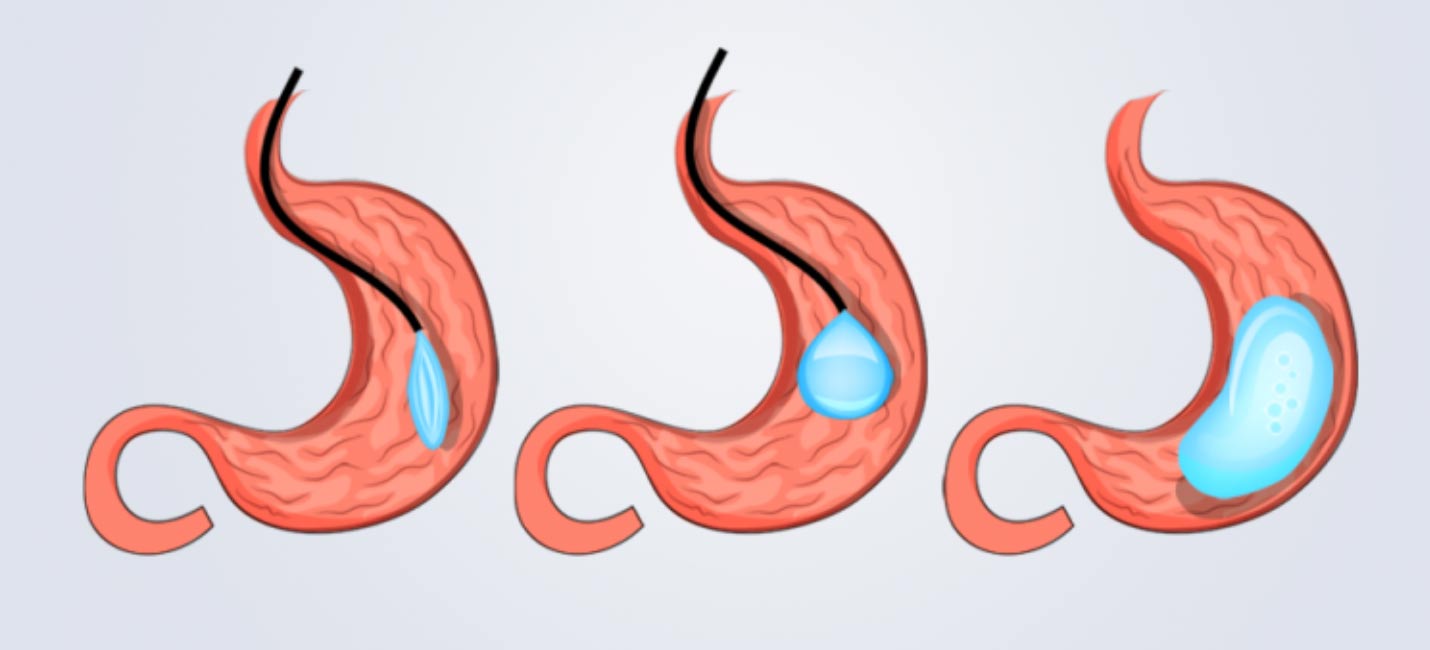
Orbera Intra Gastric Balloon
This is generally recommended for Class 1 obesity patients, who wish to lose 10-20kg, and is popular after pregnancy weight gain. It involves an inflatable silicone balloon being placed in the stomach endoscopically in a twilight sedation procedure.
The procedure generally takes around 20 minutes. BMI requirement for the Gastric Balloon is 27.0 kg/m2 or above.
Pros
- Temporary – the gastric balloon gets removed after 6-12 months, training the brain to eat less in the long-term.
- Ideal for smaller amounts of weight loss.
- Minimally invasive.
- Overnight hospital stay, back to routine next day. Healing time is 3 to 4 days.
Cons
- Weight loss is highly variable (in my patients it has ranged from an average of 10-15kg).
- For severely obese patients other surgeries may be more suitable.
- However, for morbidly obese patients, the balloon can be used as a preliminary procedure to help patients lose weight before surgery in order to reduce liver volume and better facilitate a bypass or sleeve surgery.
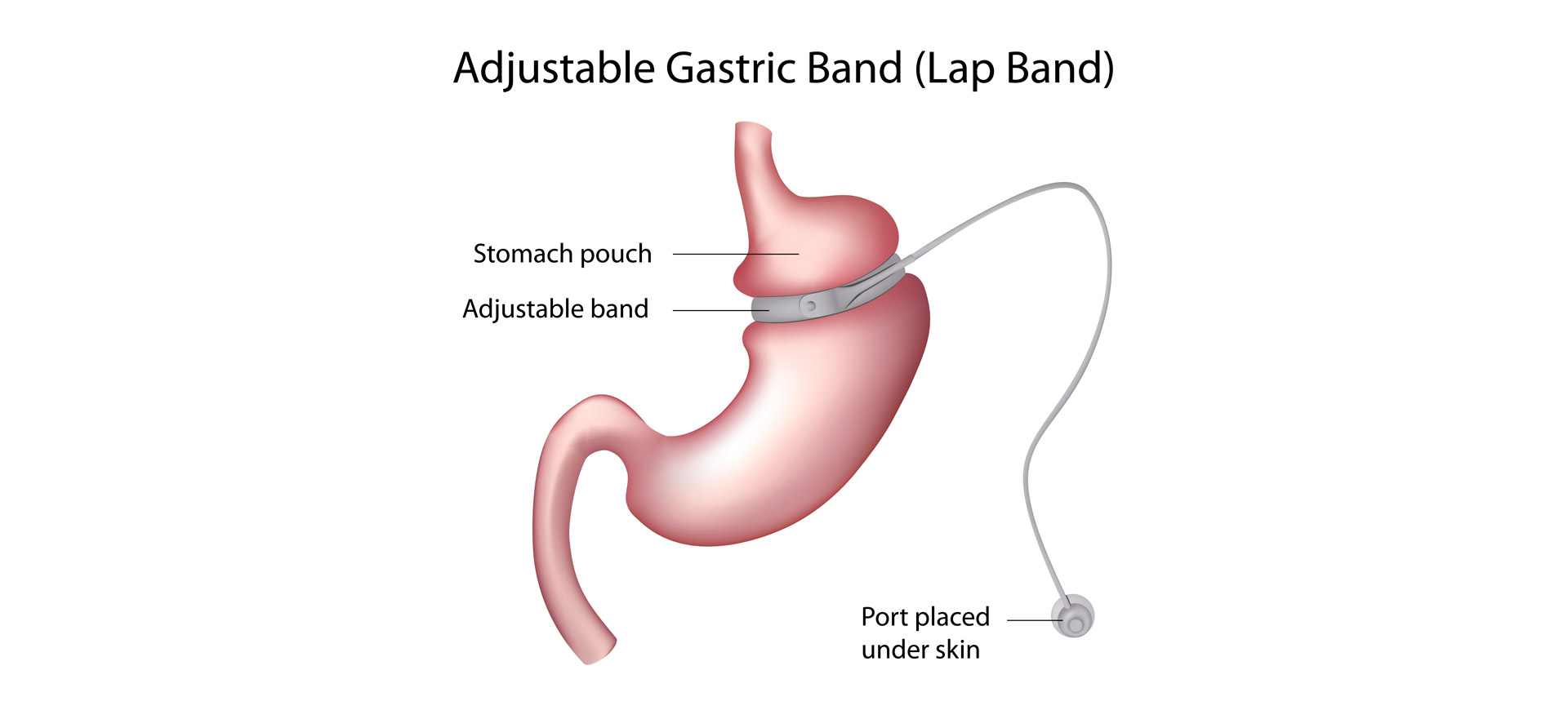
Laparoscopic Adjustable Gastric Banding (LAGB)
An adjustable gastric banding procedure uses a hollow band made of special material that is placed around the stomach near its upper end, creating a small pouch and a narrow passage into the larger remainder of the stomach. The band is then inflated with saline, and it can be tightened or loosened over time to change the size of the passage by increasing or decreasing the amount of saline.
Pros
- Minimally invasive, less complications than sleeve or bypass – similar to balloon.
- In recent years, many doctors suggested (LAGB) may not be effective as Laparoscopic Gastric Sleeve (LGS) sleeve.
- Why? Because as part of the larger part of the stomach is removed in other bariatric surgeries, satiety is also suppressed.
- With lap band surgery, the hormone that causes the need for more food is still there, and there is just a mechanical band placed around the stomach.
- However, as a surgeon who performs most bariatric procedures, I find that there is still a subset of patients who can benefit from LAGB. This includes patients who cannot tolerate metabolic surgeries, as well as patients who prefer an adjustable and reversible procedure.
- In these patients, quite often, when they get used to the new size of the stomach, it can result in lower likelihood of weight gain.
- The long-term success of LAGB has also recently been vindicated in a large Italian study published in October 2021, comparing 75 patients in each arm. It found that while the LGS achieved greater weight loss at 1 and 5 years, by 10 years the weight loss was equal in LGS and LAGB groups.
Cons
- Some studies suggest a higher revision rate. A 10-year study of 40,994 bariatric surgery patients found that laparoscopic adjustable gastric banding had a revision rate of 26%, while Gastric Sleeve had a rate of about 9.8%, as reported in the Journal for Surgery and Obesity Related Diseases found.
- However, O’Brien et al, published their 20-year results of 8,500 patients in 2018 with revision rates of only 5-10% for the band.
- Complications include port leakage or displacement, band slippage/pouch formation or erosion.
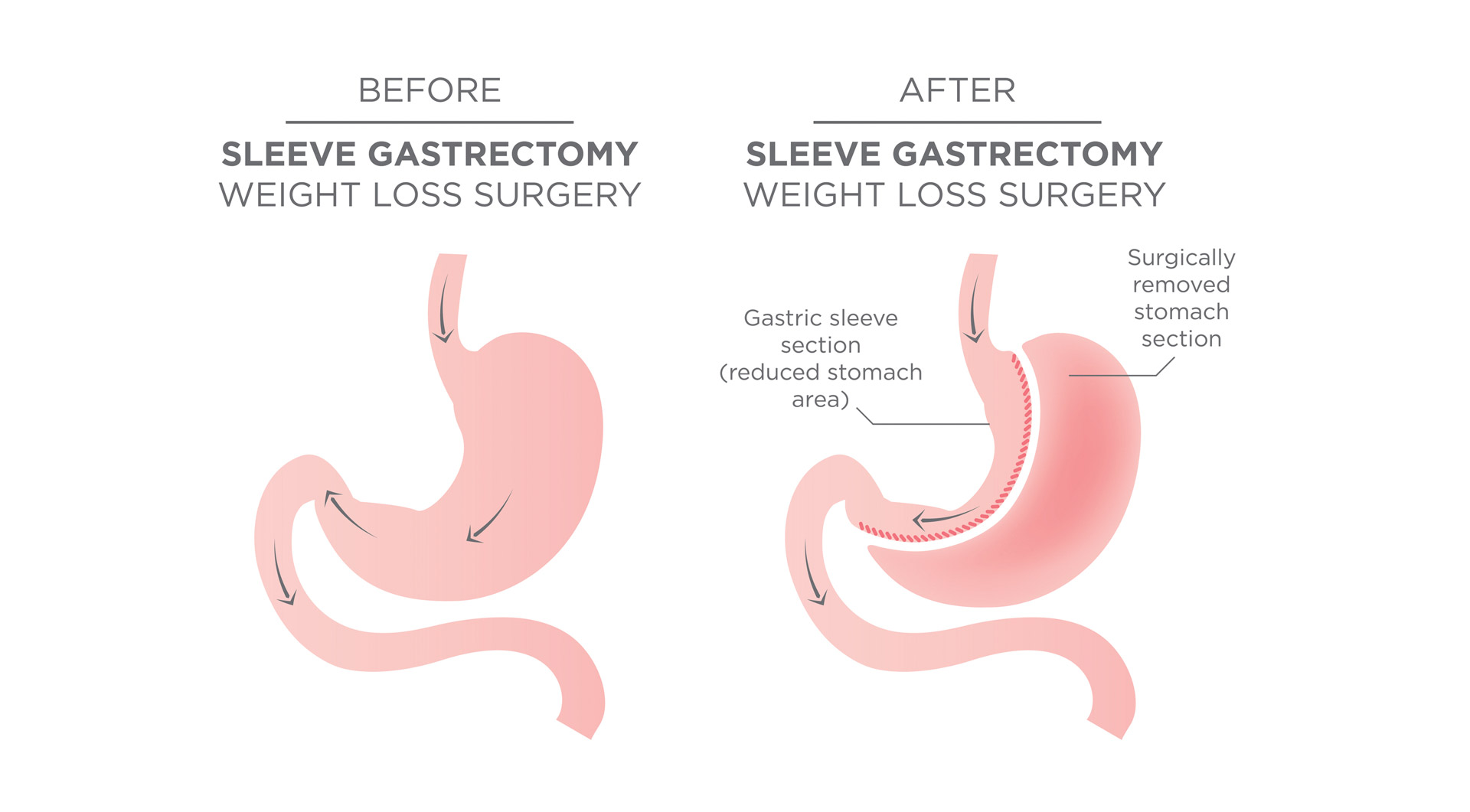
The Gastric Sleeve (Laparoscopic Sleeve Gastrectomy or LSG)
The “sleeve” is the gold standard of surgery for most uncomplicated bariatric patients.
This procedure involves removing 75% of the stomach and converting to a banana shaped sleeve. The LSG reduces appetite significantly by changing metabolic drivers in the brain.
BMI requirements changed in 2022 for the first time in 30 years, and the recommendation for Sleeve Surgery is now a BMI of 30 with co-morbidities (e.g. diabetes, hypertension or sleep apnoea) and 35 with no co-morbidities. Which means that more Australians are eligible for bariatric surgery than ever before.
Currently the Gastric Sleeve is the most popular bariatric procedure in Australia.
Pros
- Less complications for super obese patients (patients who weigh more than 180kg), when compared with gastric bypass or duodenal switch.
- Shorter time under general anaesthesia, 40–50-minute operations
- Only 2-3 days in hospital, healing time two weeks, return to routine in three weeks.
- Less chance of dumping syndrome (which causes diarrhea, nausea after meal).
- Considered safe for many patients with bipolar or schizophrenia, which in decades past were contraindicated.
- Many patients can go off diabetes medications and blood pressure medications after surgery.
Cons
- Not reversible (but can be converted to a bypass).
- Less suitable for patients with reflux.
Gastric Bypass Surgery (Roux-en-Y Gastric Bypass)
In the Gastric Bypass procedure, a small stomach pouch is created to restrict food intake.
The next stage of the operation involves a Y-shaped section of the small intestine being attached to the pouch to allow food to bypass the lower stomach, the duodenum (the first segment of the small intestine), and the first portion of the jejunum (the second segment of the small intestine).
This bypass reduces the absorption of nutrients and thereby reduces the kJ intake and increases satiety. Like sleeve surgery, this is a “metabolic” surgery that also impacts the brain’s hunger drivers.
New BMI requirements for Gastric Bypass Surgery are now 30 with co-morbidities (e.g. hypertension, sleep apnoea or diabetes) and 35 with no co-morbidities. This means more patients meet the eligibility criteria for Bypass.
Pros
- Generally achieves the most and fastest weight loss of all bariatric surgeries.
- The procedure is potentially reversible.
- More suitable than LSG for some people with diabetes and reflux.
- Now considered safe for many patients with bipolar or schizophrenia, which in decades past were usually contraindications for bariatric surgery.
- Like the sleeve, many patients can go off diabetes and blood pressure medications after surgery due to metabolic changes in brain hormones.
Cons
- More issues with nutrient absorption.
- Usually requires a longer anaesthetic time of 2-4 hours.
- Hospital stay: 3-5 days. Healing: 2 weeks. Return to routine: 3 weeks – 2 months.
- More chance of dumping syndrome than with sleeves.
Points to remember
- Surgery is often marketed as a physical “makeover”; however, the health benefits are lifesaving.
- If you are obese and have other co-morbidities, especially, the potential benefits of bariatric surgery in terms of improving your quality of life and reducing the risks of cancer, asthma, diabetes, hypertension, and cardiovascular events far outweigh any associated risks.
- Surgery outcomes have significantly improved based on 30 years of data and low morbidity and mortality annually (about 0.03 to 2% annually) in a cohort of patients that most certainly face premature death and significant morbidity.
- Procedures used to take 2-4 hours, now procedure times range from 15 minutes to 90 minutes.
- While there are presently no absolute contraindications to bariatric surgery, relative contraindications for the more extensive surgeries such as sleeve and bypass do exist including heart failure, unstable coronary artery disease, end-stage lung disease, drug and alcohol dependency, impaired intellectual capacity and Crohn’s Disease (for Bypass).
- At the Winnett Specialist Group, patients are seen by both myself and dietitians twice pre-operatively, as well as specific specialists such as cardiologists, respiratory physicians, endocrinologists, clinical psychologists and/or psychiatrists as required.
- All patients will receive dietetic and psychological support throughout their weight loss journey at Winnett Specialist Group.
Mr Jason Winnett
Laparoscopic and Bariatric Surgeon
P (03) 9417 1555 admin@winnettspecialistgroup.com.au
www.winnettspecialistgroup.com.au
Queens Terrace, 382 Victoria Parade, East Melbourne 3002



